Definition
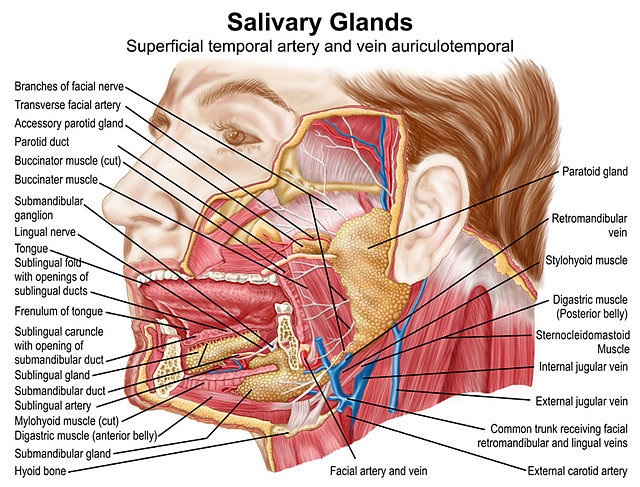
Submandibular glands are the second-largest salivary gland type, producing around 65% of our saliva when unstimulated (at rest). Located under the jaw, the exocrine submandibular glands empty under the tongue, just behind the lower front teeth, via the Wharton duct. Both submandibular glands receive parasympathetic input via the chorda tympani nerve and take a secondary role to the parotid in the presence of stimulation.
Submandibular Gland Function
Submandibular gland function is solely to contribute to the production and delivery of saliva. The three human salivary glands (parotid, submandibular, and sublingual) produce up to 1.5 liters of saliva every day. Saliva has many different functions in the oral cavity and will be discussed further on.

It is, therefore, more appropriate to concentrate on the production and actions of saliva when discussing submandibular gland function. First, let’s look at saliva production and the ways in which specialized cells form different elements of ‘whole’ saliva.
All three salivary glands contain three important cell types. These are the acinar cells, ductal cells, and myoepithelial cells. Similarly, all of these three salivary glands consist of a similar structure of three types of ducts that join and open into the oral cavity.
The acinar cells are responsible for saliva production. The rule of three applies here, too, as there are three main types of acinar cell: serous, mucinous and seromucous (mixed). Serous acini produce a watery secretion packed with proteins that are stored as zymogen granules. Mucinous acini store a much thicker secretion rich in specific glycoproteins known as mucins. When extracted from the cell through the action of the myoepithelial cells (see below), this mucin-rich substance mixes with the watery excretion of the serous acinar cells to form saliva. As you probably realize, seromucous acinar cells produce both serous and mucinous secretions.
Myoepithelial cells surround the acinar cells (pl. acini) and ducts, contracting at regular intervals and squeezing saliva from the acinus and pushing saliva into the oral cavity via the ducts when stimulated by the autonomic nervous system. An acinus refers to a group of acini. Each acinar cell group is also ringed by an extracellular matrix, nerve fibers, and other cell types including immune cells.
The submandibular glands produce predominantly serous saliva as only around 10% of submandibular gland acini are mucinous. The image below shows the structure of a generic tubuloacinar gland with the ductal cells colored in purple and the acinar cells in green. The larger, rounder acinar cells are serous and the smaller, more straight-edged cells are mucinous.
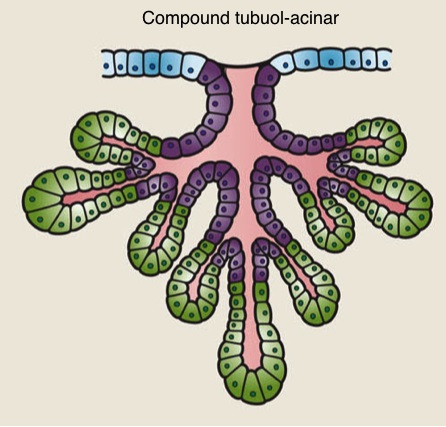
The salivary ductal system is not merely a route for saliva transportation into the oral cavity. As acinar cell secretions pass through the system of ducts their electrolyte content is adjusted. Just like acinar cells, ductal structures are also classified into three different types. These are intercalated, striated and excretory ducts.
Intercalated ducts exit immediately from the acini and allow bicarbonate to be added to the secretion in return for chloride. Intercalated ducts then empty into striated ducts that reabsorb sodium and add potassium. The largest duct, the excretory duct, further regulates electrolyte balance by way of osmosis.
The Function of Saliva
This function of saliva covers various aspects of digestion, lubrication, and protection. It is a clear, slightly acidic exocrine secretion produced by the three major salivary glands as well as the minor labial, buccal, glossopalatine, palatine, and lingual salivary glands. A further source of the constituents of saliva comes from gingival crevicular fluid or secretion that arises from the areas around the gums.
Saliva is 99% water. The other 1% is a combination of sodium, potassium, calcium, magnesium, bicarbonate, phosphate, immunoglobulins, proteins, enzymes, mucins, urea and ammonia. These ingredients give many indications of saliva function. When unstimulated and controlled by the parasympathetic nervous system, the submandibular glands produce the most saliva of which the majority is watery. When stimulated by the sympathetic nervous system in the thought, presence, sight or smell of food, for example, the parotid glands become dominant and saliva contains higher quantities of proteins.
Saliva acts as a buffer according to its level of acidity (5.3 – 7.8 pH). The bicarbonate, phosphate, certain peptides and urea in saliva are able to modulate its pH.
Proteins and mucins act to gather oral microorganisms in groups. Dental plaque is part of this process, where the adhesive characteristics of the protein, mucin and bacterial, fungal and viral mix coat the enamel of the teeth. Mucins are very sticky and viscous complex protein molecules that lubricate the entire oral cavity, aiding chewing, swallowing and even speech. Two types of mucins are produced in the submandibular gland – MG1 and MG2. The former sticks to tooth and tissue surfaces to help protect them, the latter also sticks but is easy to displace, gathering bacteria and taking them into the highly acidic environment of the stomach upon swallowing where these potentially harmful bacteria are usually unable to survive or colonize.
Some proteins, and calcium and phosphate can stop a number of components from dissolving into the watery saliva and so aid tooth remineralization and prevent dental demineralization.
Salivary immunoglobulins, some proteins, and enzymes are antibacterial in action. The immunoglobulins IgA, IgG, and IgM are found in large quantities in our saliva, the majority of which consists of IgA which is permitted to enter through salivary gland ductal cells. It is supposed that IgG and IgM are introduced via the gingival crevicular fluid. Nonimmunogenic ingredients that help fight pathogenic bacteria, viruses and fungi are proteins, mucins, peptides, and enzymes. The latter of this group is composed of products such as lactoferrin and peroxidase which are produced by the acinar cells. In addition, the glycoprotein known as MG1 mucin works much better in the presence of immunoglobulins. Some enzymes bind with potential bacterial food sources (nutritional immunity), others attack bacterial cell walls, others poison the bacteria. In addition, other proteins adhere to bacteria, forming clumps that can either be more easily swallowed or destroyed by the immunogenic and nonimmunogenic saliva contents.
Because saliva is hypotonic when it exits the excretory ducts it also allows the taste buds of the tongue to sense taste. Water is necessary to taste food and saliva provides a medium in which food flavors and aromas can dissolve. Saliva hypotonicity also allows mucin particles to absorb water and expand. While mucus lubricates, it also provides a protective covering to the inner membranes of the oral cavity, protecting it from irritants in the form of chemicals (smoking, dental plaque) and from drying out when breathing through the mouth.
The most recognized function of saliva is its role in digestion; however, this role is a minor one. The enzyme amylase (produced in the parotid gland) helps break up starch molecules, although the brunt of this task is relegated to the amylases produced by the pancreas after chyme has passed through the stomach. Lipases in the saliva help to break down triglycerides. Yet the primary function of saliva in early digestion is simply to lubricate the food bolus and so make the act of swallowing an easier one.
Swollen Submandibular Gland
Swollen submandibular glands are not to be confused with swelling in other salivary glands. Inflamed parotid glands can be felt in front of the ears. Sublingual glands sit under the tongue and are not easy to palpate but when swollen can be felt by the patient when moving the tip of the tongue over this area.
It is easy to confuse a swollen gland with a swollen lymph node. Lymph nodes are scattered all around the salivary glands and can make diagnosis difficult. In the case of enlarged submandibular glands, one should palpate under the inferior border of the mandibular body, close to the angle of the jaw.
Salivary gland disorders are caused by conditions that either affect the gland tissue to its associated ducts. Gland tissue swelling and inflammation may be the result of a viral infection, benign lymphoepithelial lesions (BLEL) or malignant lymphoepithelial lesions (MLEL). Anomalies in the saliva or its drainage might be the result of acute dehydration, stenosis (duct constriction) or sialectasis (duct dilation), for example. Calcium-stone formation (calculi) due to the high mineral content of saliva is possible, and these stones may block the flow of saliva from gland to oral cavity where stagnation increases the risk of infection and subsequent inflammation.
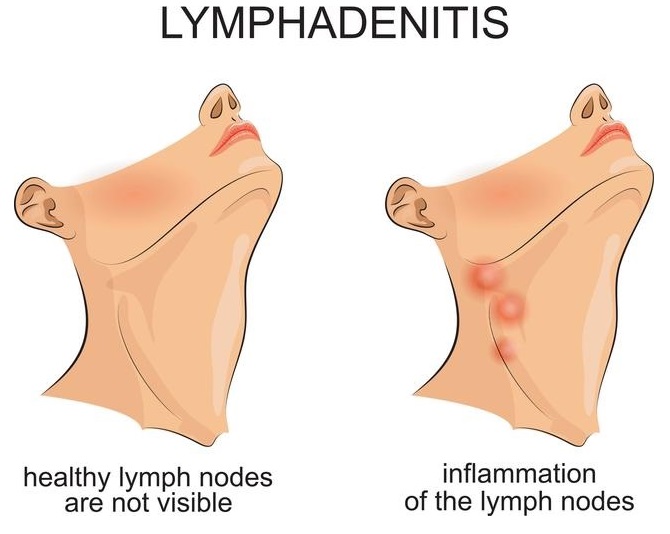
Most cases of submandibular gland swelling are acute and when associated with fever and pain may be the result of sialolithiasis (salivary gland stones) or sialadenitis (bacterial or viral infection of the gland).

Chronic generalized swelling on both sides and with little or no associated pain may indicate sialoadenosis (sialosis) which is not an inflammatory reaction but gland enlargement and more likely to be found in alcoholics with liver disease and diabetics, and in malabsorption or malnutrition scenarios. When in combination with a dry mouth other systemic causes may be human immunodeficiency virus and Sjögren’s syndrome.
Long-term swelling of a single major salivary gland can also be the result of salivary stones and bacterial or viral infections such as the mumps. Soft and tender lumps at or very close to the gland may be caused by a mucal cyst (ranula). Other causes may be autoimmune disorders, cuts and scratches, and dental and upper respiratory tract infections.
Tumors in the submandibular area are relatively rare but patients over 40 years of age presenting with a palpable, non-tender, slightly hard and chronic submandibular lump should be further investigated and may require surgery.

Submandibular Gland Pain
Submandibular gland pain is usually the result of pressure caused by a blocked duct or nerve pain where a benign or malignant tumor presses onto a nearby sensory nerve. Salivary gland disorders that cause pain are most usually sialolithiasis or salivary gland stones. Sialolithiasis describes the deposition of very small, calcium-rich stones that can become trapped either within the gland or its associated ductal network. Sialolithiasis may be the result of long-term dehydration, starvation (where less saliva is produced with less saliva flow), and certain types of medications.
When a duct becomes blocked by a calculus both pain and swelling occur as saliva flow completely or partially comes to a standstill. Saliva trapped behind the stone stagnates and is susceptible to infection. Bacterial, fungal or viral infection of the salivary gland is called sialadenitis and is a similarly painful and swollen condition.
Systemic infections can cause swelling in all of the salivary glands. Specific submandibular symptoms are swelling under the jaw and pain when eating.
Noncancerous or benign tumors are most commonly found in the parotid gland. While cancer does occur in the salivary glands this is rare; it usually responds to treatment. Sjögren syndrome is a risk factor, as is smoking and exposure to radiation.
Submandibular Gland Anatomy
Submandibular gland anatomy is not complicated. Blood supply is provided by way of a branch of the carotid artery known as the facial artery (indicated by the green arrow in the below image) and toxins and carbon dioxide are removed via the facial vein.
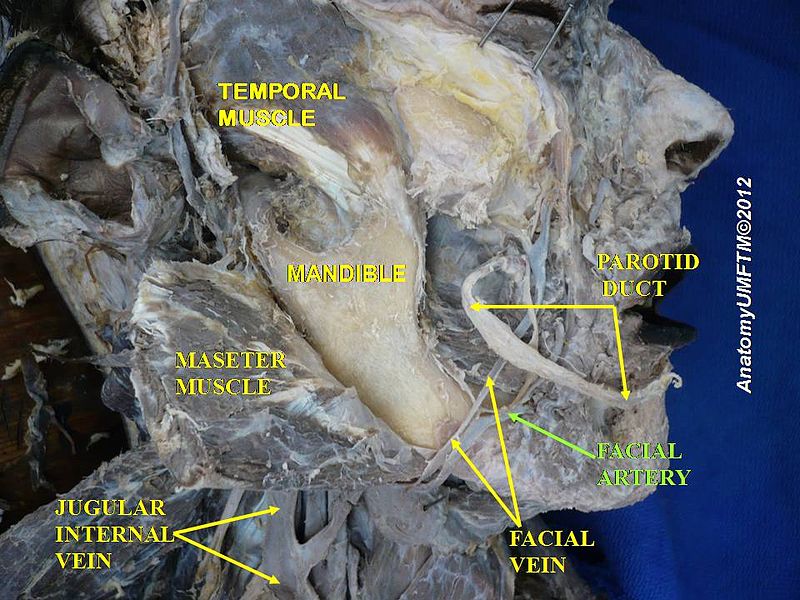
The submandibular glands are found under the mandible and between the loops of each digastric muscle (pictured below). These glands have a smaller anterior lobe and a larger posterior lobe. Wharton’s duct enters the oral cavity along the tongue frenulum, close the hypoglossal nerve.
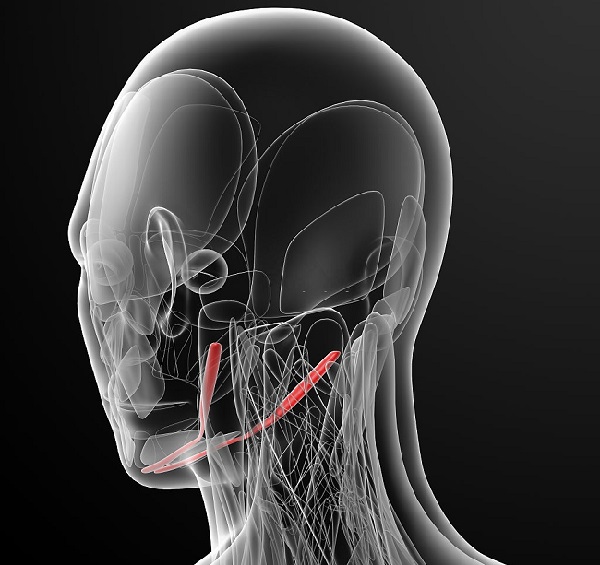
It is possible to feel the submandibular gland through the location of the submandibular triangle, the edges of which are made up by the anterior belly of the digastric muscle, the posterior belly of the digastric muscle and the inferior border of the mandibular body (the ridge of the lower jaw). The submandibular glands sit in a U-shape form over the digastric muscle bellies and can, therefore, be palpated, although not without practice as a portion lies under the bone of the mandible.
Once again, the number three is associated with this part of the anatomy. The submandibular gland has three layers or surfaces. The inferior surface is covered by the skin and the platysma muscle. The lateral surface of the submandibular gland that sits just under the mandible and the medial surface is found under the tongue and the posterior bellies of the digastric muscles.
Parasympathetic nerve fibers from the chorda tympani travel in the lingual nerve and synapse in the submandibular ganglion. Once the ganglion has been reached, a percentage of postganglionic nerve fibers enter the submandibular gland and the others take a longer route by way of the lingual nerve. Stimulation of the parasympathetic nervous system by way of the neurotransmitter acetylcholine increases saliva secretion by the acinar cells, increases bicarbonate absorption in the ductal cells and causes the myoepithelium to contract at more regular intervals.
Sympathetic fibers travel to the submandibular ganglion via the superior cervical ganglion. Sympathetic stimulation through the neurotransmitter noradrenaline lowers the amount of saliva produced by acinar cells but increases the amount of protein in the produced saliva. In addition, blood flow to all salivary glands is reduced.
Quiz
