Lipolysis Definition
Lipolysis is the process by which fats are broken down in our bodies through enzymes and water, or hydrolysis. Lipolysis occurs in our adipose tissue stores, which are the fatty tissues that cushion and line our bodies and organs. In fact, fats can be thought of simply as stored energy. Fats are ready and available for when our glucose stores run low between meals, and it makes sense for lipolysis to occur as it will facilitate the movement of these stored fats through our bloodstream. Breaking down this “potential energy” into free moving fatty acids can then allow them to be repurposed or expended as fuel!
Lipolysis actually has links to various processes within our bodies. Free fatty acids are vital cell-to-cell communicators, are a staple ingredient of gluconeogenesis and cellular respiration, and can upregulate the transcription of proteins like the uncoupling proton channels that line our mitochondrial membrane – which will inhibit ATP synthesis without disrupting the respiratory chain. In sum, lipolysis is a key life-sustaining biological process; although, as of late, it’s taken on new meaning at cosmetic clinics around the world for its promise to zap unwanted fat! While for their namesake, both processes technically “lyse” or break fats, the way in which they accomplish this is obviously different – the latter utilizing cool lasers or heat to reduce fat cells.
Lipolysis Mechanism
Triglycerides are undoubtedly the main energy molecule in eukaryotic cells. Triglyceride is a glycerol derivative that is stored as lipid droplets within our fatty tissues, and herein lipolysis takes place. Let’s begin by describing lipolysis in big picture scope. These lipid droplets are first targeted by lipolytic enzymes that are highly regulated and will access these droplets in the event of phosphorylation.
These lipases will ensue to sequentially hydrolyze our triglycerides into their glycerol and fatty acid components until we are left with sole glycerols, and this takes place with three enzyme reactions. The breakdown of fats is termed beta-oxidation, or “fatty acid” oxidation because the triglycerides are being oxidized into their most basic functional parts. We are thus left with free fatty acids and glycerol that can enter other metabolic pathways or find new purpose. Let’s dive into specifics.

The image depicts the Lipolysis mechanism, breakdown of triglycerides into fatty acids and glycerol.
The first and rate-limiting step of lipolysis involves the enzyme, adipose triglyceride lipase (or ATGL), which is sensitive to hormones. The ATGL will hydrolyze our triacylglycerol into a diacylglycerol, losing a free fatty acid that will be free to mobilize in our bloodstream. The resultant diacylglycerol will then be acted upon by hormone-sensitive lipase (HSL), which will remove another fatty acid to give a monoacylglycerol molecule. Finally, monoacylglycerol lipase (MGL) will break the monacylglycerol further down to a single glycerol molecule.
The figure below illustrates the main “destinies,” if you will, of the resulting fatty acids and glycerol. Fatty acids can undergo beta-oxidation and repurpose to create Acetyl-CoA. Of course, Acetyl-CoA is best known as a vital starting molecule that initiates the Krebs’s cycle in cellular respiration. This repurposing is vital when glucose stores are low in times of starvation, or even between meals, as cellular respiration can continue to run and sustain life. Similarly, the free glycerol can enter glycolysis. Normally glucose is converted to G6P at the first step of glycolysis. In the event that glucose levels are low, glycerol will be converted to dihydroxyacetone phosphate and will enter glycolysis at the second control point to keep glycolysis running. Thus, fats make the best energy store as they will ensure that cellular respiration continues to run and ATP is produced.
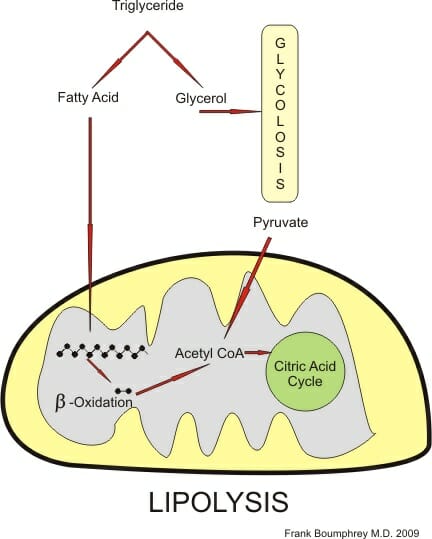
The figure illustrates Lipolysis and the pathways the fatty acids and glycerol components take.
Lipolysis Regulation
Like every vital biological process, lipolysis is regulated to meet our needs. At any given time, it would be extremely harmful to have tons of free fatty acids flowing through our bloodstream. Anyone with high cholesterol or arterial plaques will attest to that. Thus, lipolysis – and its inverse process, lipogenesis – need to be counter-regulated and highly sensitive to the levels of specific hormones and proteins. For example, stimulatory hormones like, epinephrine, norepinephrine, cortisol, glucagon, and growth hormone induce lipolysis. Key hormones glucagon and epinephrine will use the same pathways to induce lipolysis with minor differences.
Both glucagon and epinephrine will serve as ligands that will bind to G-protein coupled receptors on the surface of fat cells. The G proteins will then activate adenylate cyclase and upregulate their conversion of ATP to cAMP. We might recognize cAMP as the famously ubiquitous secondary messenger of so many other biological pathways. Likewise, here the cAMP will activate protein kinase A (PKA), which will expend an ATP molecule in phosphorylating and upregulating the hydrolysis activity of our HSL enzyme – otherwise known as our second enzyme in the lipolysis pathway. As a result, we are left with free fatty acids and glycerol that can then enter metabolic pathways to counter the low sugars in our blood, for instance. Understandably, HSL was thought to be the rate-determining enzyme of lipolysis for some time before TAG lipase (or ATG, our first enzyme) was uncovered to be the key initiative lipolytic step. Let’s quickly take a look at why it makes sense for glucagon and epinephrine to trigger lipolysis.
Glucagon-induced Lipolysis
Glucagon is a peptide hormone that is synthesized by pancreatic cells in the event that glucose and thus insulin levels drop. Glucagon will then trigger our liver to break down its glycogen stores and release much needed glucose into our blood. Conversely, when our glucose and insulin levels are high, insulin in healthy individuals will allow glucose to exit the bloodstream and be taken up by insulin-dependent tissues. Of course, in diabetics, the tissues will no longer respond well to insulin and this sugar will not reach the tissues and instead cause havoc in the bloodstream.
Shifting back our focus to lipolysis, glucagon stores are small and will be expended quickly. Fat stores, on the other hand, are vast and ready to use. Here, glucagon serves its key role. Glucagon will bind to Glucagon G-protein coupled receptors on fat cell membranes, and trigger the HSL-activating pathway described earlier. The glycerol that is released can then travel to the liver or kidney where it will be eventually converted to GA3P and enter glycolysis and our gluconeogenesis pathway to synthesis badly needed glucose (refer to figure 2).
Epinephrine-induced Lipolysis
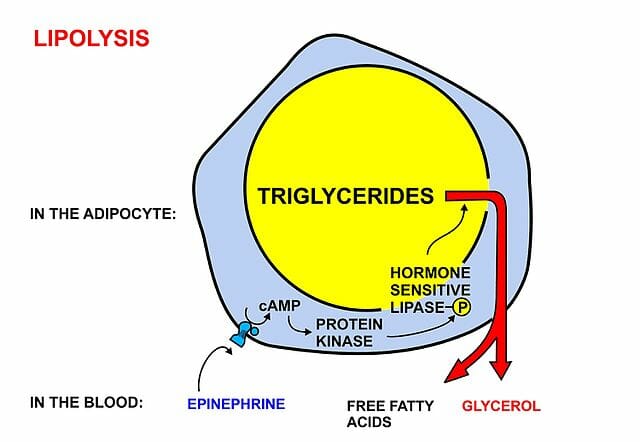
The diagram specifically illustrates epinephrine-induced Lipolysis through a G-protein mediated pathway.
Epinephrine will also bind G-protein receptors on fat cell membranes, however they will specifically bind beta-adrenergic receptors. This binding will likewise lead to the cAMP/PKA-led phosphorylation of hormone sensitive lipase, that will ultimately drive the release of free fatty acids and glycerol. Epinephrine is known for its connection to our instinctual “fight or flight” response. This hyperarousal occurs when we perceive an attack or threat to our survival. Thus, it makes sense that epinephrine would trigger lipolysis and its resulting up-drive of metabolic processes. If we are ever starving, our body will certainly react to this threat and use our fatty energy stores to respond and sustain life at all costs.
Lipolysis in Popular Culture
As briefly mentioned above, a fun fact is that lipolysis has become a popular term in the cosmetic world. Not to be confused with the adipose lipolysis pathways detailed in this article, laser lipolysis and even injection lipolysis are clinically proven methods of reducing the number of fat cells without liposuction surgery. Noninvasive fat reduction has become a new cosmetic staple, and promises to target fat cells through the use of heat, cooling (via lasers or radiofrequencies), or less commonly deoxycholic acid injections without disrupting surrounding tissues.
Quiz
1. Which of the following enzymes is the rate determining enzyme in lipolysis?
A. HSL
B. ATGL
C. MGL
D. None of the above
2. Which of the following will induce lipolysis?
A. High insulin/Low epinephrine
B. High insulin/High epinephrine
C. Low insulin/High epinephrine
D. Low insulin/Low epinephrine
References
- Binienda, Z et al. “Role of Free Fatty Acids in Physiological Conditions and Mitochondrial Dysfunction.” SCIRP: Food and Nutrition Sciences, Vol. 4 No. 9A, 2013. Retrieved <http://www.scirp.org/journal/PaperInformation.aspx?PaperID=36092>
- American Society of Plastic Surgeons (2018). “Nonsurgical Fat Reduction: Minimally Invasive Procedures.” Plasticsurgery.org. Accessed 2018, May 29 from <https://www.plasticsurgery.org/cosmetic-procedures/nonsurgical-fat-reduction/laser-lipolysis>
- Ward, Colin (2015). “Lipolysis and Lipogenesis.” Diapedia: 51040851148 rev. no. 17. Accessed 29 May 2018 from <https://www.diapedia.org/metabolism-insulin-and-other-hormones/51040851148/lipolysis-and-lipogenesis>
- Engelking, Larry R. (2014). “Chapter 70 – Lipolysis.” Textbook of Veterinary Physiological Chemistry (3rd Edition), Pages 444-449. Accessed 30 May 2018 from <https://www.sciencedirect.com/topics/neuroscience/lipolysis>
- Fruhbeck, G et al. “Regulation of Adipocyte Lipolysis.” Nutr Res Rev. 2014 Jun; 27(1): 63-93. Doi: 10.1017/S095442241400002X
