Definition
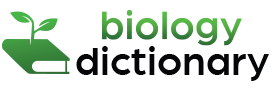
The urinary system produces, stores, and excretes urine via a filtration mechanism in which potentially harmful molecules are removed from the body. It also plays a crucial role in water homeostasis, electrolyte and acid-base balance, and red blood cell production.The human urinary tract is comprised of two kidneys, two ureters, one bladder, two sphincters, and one urethra.

How Does the Urinary System Work?
How the urinary system works is relatively simple, although the supplementary roles of the kidneys can be complex.
Blood is transported to the kidneys via the renal artery. A system of filtration units within the kidney regulates levels of dilution (water), salts and other small molecules in the filtrate. Any excess or undesired products travel through each ureter and are deposited into the reservoir of the bladder, while purified blood re-enters the circulatory system by way of the renal vein. Urine is stored in the bladder until the urinary nervous system releases the contents through the urethra and out of the body. The passing of urine is known as micturition or urination.
The urinary system is split into the upper and lower urinary tract. The former consists of the kidneys and ureters, the latter of the bladder and urethra.
How much urine is expelled depends on various factors: the ratio of waste products to water, dietary habits, physical activity levels, medications, comorbidities, and the state of health of various organs and systems within the body.
Urinary System Function
The main urinary system function is to filter the blood of excess water, salts, and waste products, temporarily store these within a reservoir, and intermittently expel these products from the body.
Filtration, Reabsorption, and Secretion
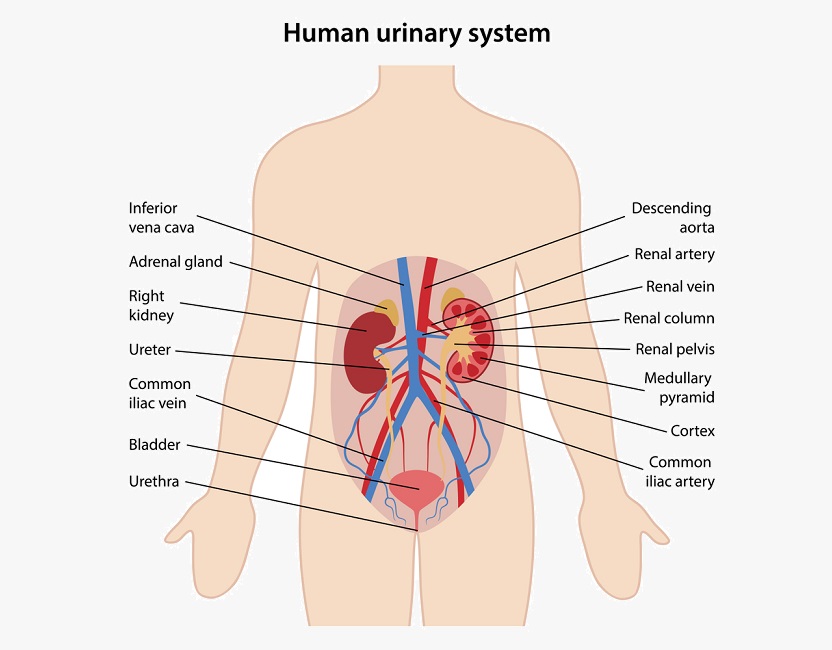
Each kidney contains approximately one million nephrons. Nephrons play a crucial role in removing waste products and adjusting concentrations of water, ions and smaller molecules in the blood. A single kidney contains enough nephrons to filter the blood and produce urine – for this reason, kidney transplants can use organs from living donors. When both kidneys are damaged, ions, salts, water, and small molecules accumulate in the body, causing complete organ failure and death if left untreated. A kidney cannot generate new nephrons – once they are damaged, they can not be replaced.
A nephron is an entire system within itself with different parts of its structure situated in different areas of the kidney. The long Loop of Henlé (some nephrons only have a short loop) can be found in the central region of the kidney – the medulla. Other structures are found in the renal cortex or outer layer. Nephrons receive a blood supply via an afferent arteriole and return filtered blood back into the circulation via an efferent arteriole. These are two ends of a long, convoluted group of capillaries which surrounds the nephron, allowing the diffusion of water, ions, salts, and other molecules. The image below shows the blood flow into the kidney and nephron (in red), the production and excretion of urine (yellow), and the return of reabsorbed products and filtered blood into the circulatory system (blue).
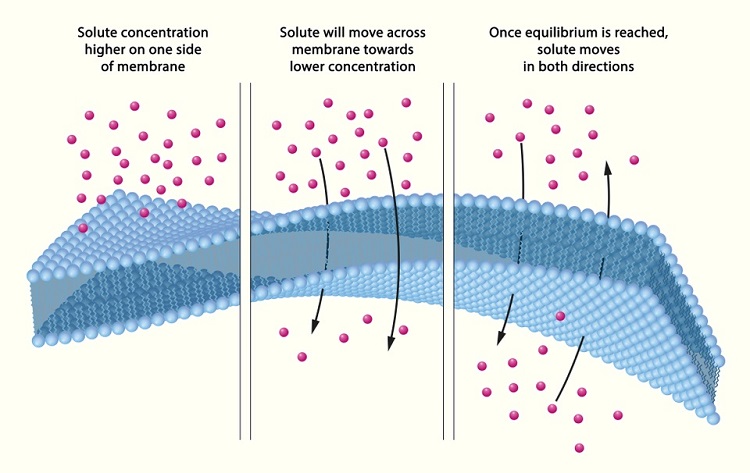
A nephron has three functions: glomerular filtration (of water and solutes within the blood), tubular reabsorption (the return of water and required molecules to the circulation), and tubular secretion (of waste or excess molecules – including water) into a distal tube. This secreted fluid is known as urine. Every minute, approximately 125 ml of blood is filtered by the nephrons of both kidneys. The majority of filtrate is reabsorbed – meaning in a period of 24 hours, around 180 liters of filtrate are produced but only 1.5 liters of this is excreted as urine. Filtration occurs within the glomerulus, tubular reabsorption in the proximal convoluted tubule, and tubular secretion in the distal convoluted tubule. The loop of Henlé maintains a concentration gradient so that water and ions are more easily reabsorbed. In the image below, the achievement of equal concentrations of a solute on either side of a membrane by the process of diffusion is depicted. Both osmosis and diffusion occur within nephrons. Osmosis is the movement of water, not solute, through a semi-permeable membrane.
Reabsorbed molecules include glucose, amino acids, sodium chloride, and water, as well as calcium, potassium, hydrogen and bicarbonate ions.
Secreted molecules are urea, uric acid, creatinine and hydrogen, and potassium ions. Uric acid is a product of nitrogenous metabolism, a mechanism that breaks down ingested purine proteins. Urea is a byproduct of ammonia which is formed in the liver, also from the breakdown of amino acids. Creatinine phosphate or phosphocreatine is a by-product of cellular energy production when adenosine triphosphate (ATP) is converted to adenosine diphosphate (ADP). In order to form another ATP molecule, an extra phosphate molecule is necessary – creatinine phosphate. The liver and kidney produce creatinine phosphate, and it can also be ingested from meat sources.
Larger molecules such as proteins and glucose are usually unable to pass into the nephron, yet in kidney diseases and their symptoms such as diabetic nephropathy or nephrotic syndrome, the glomeruli of the nephrons leak and large molecules and even blood cells can be found in the ultrafiltrate (urine). For this reason, the protein content of urine is often measured in at-risk patients such as diabetics and pregnant women. A simple urine test strip will indicate levels of various large cells or molecules within the urine, including white blood cells, proteins, ketones, and glucose.

Urine Transportation and Storage
Nephrons empty the final product – urine or ultrafiltrate – into a system of collecting ducts which bring the urine into the ureter. Ureters are two narrow but relatively long tubes (approximately 25 – 30 cm) which leave the kidneys and enter the urinary bladder. Ureter muscle layers help by way of peristalsis – the involuntary contraction and relaxation of smooth muscle – to propel urine towards the urinary bladder. Gravity also plays a part.
The function of the urinary bladder is to store and expel urine. Once the urine is transported into the bladder it does not flow back due to directional forces of the ureter muscle layers and the flattened ends of the ureters where ureter and bladder meet (the vesicoureteral junction). This flattening increases as the bladder fills, making it difficult for urine to flow back towards the kidneys. However, this can occur in cases of vesicoureteral reflux due to anatomical abnormalities in ureteral positioning at the vesicoureteral junction or in nerve disorders where peristalsis and muscle tone are affected.
Micturition
A human bladder usually stores around 300 to 600 ml of urine before micturition and is controlled by the pontine micturition center of the brain.
The triangular shaped bladder is a large muscle into the top of which the two ureters empty the urine. Under the bladder, close to where it connects to a single urethra, lie two circular sphincters – internal and external. These only relax during micturition and otherwise prevent urine from constantly leaking out. The internal sphincter is an involuntary muscle; the external sphincter is voluntary. The urinary bladder is lined by a thick mucosa which forms folds when the bladder is empty but opens out as the bladder fills and expands.
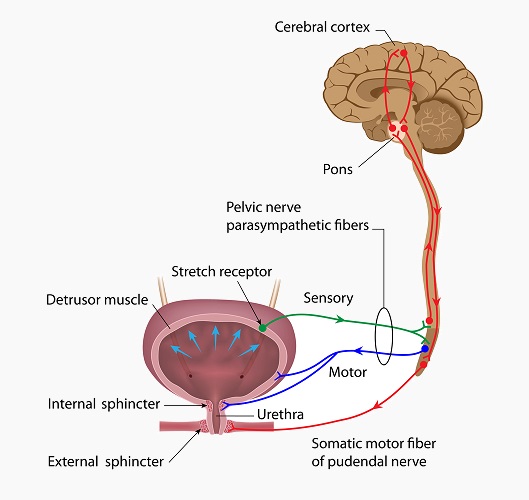
Located within the bladder wall are stretch receptor cells. When the bladder fills to around 250 ml, the mucosal folds open and stimulate these stretch receptors. They send signals to the pontine micturition center of the brain. The brain responds by relaxing the internal urethral sphincter. The external urethral sphincter remains closed until the person in question chooses to urinate, although in babies, the elderly, and those with motor or sensory nerve disorders such as sufferers of multiple sclerosis, this is not always a voluntary action.
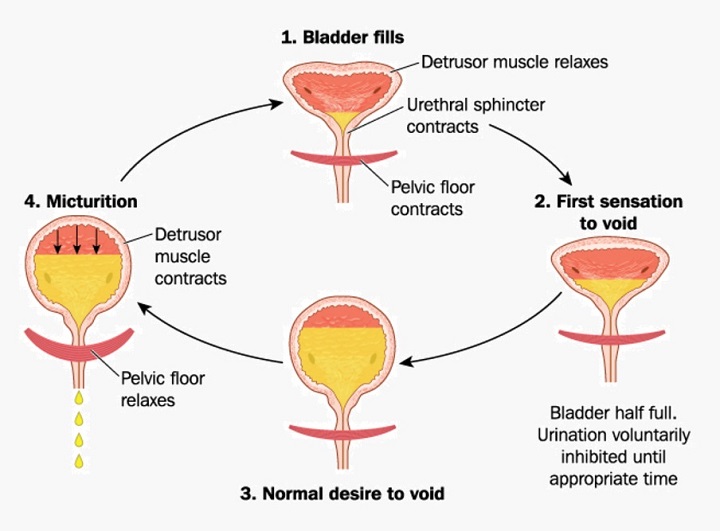
Upon relaxation of the voluntary external sphincter, urine from the bladder flows through the urethra and is expelled from the body. The image below shows the stages of micturition and the muscles involved, namely the detrusor muscle of the urinary bladder, the internal urethral sphincter, and the pelvic floor muscle which surrounds the external sphincter.
Urinary System Organs and Urinary System Structures
The main urinary system organs and other urinary system structures are the kidneys, bladder, ureters, and urethra. These form a sterile environment which is protected against the non-sterile outside world, provide the forces necessary to expel urine through a series of organs, and respond to sensitive involuntary and voluntary nervous stimulation.
Kidneys
Kidneys are located just below the ribs and are close to the middle of the back. They have multiple functions. The kidney creates balance in the amount of water and electrolytes in the body’s circulatory system, removes waste products (including drugs) from the body, controls blood pressure through the release of hormones (RAAS), regulates red blood cell production and subsequent tissue oxygenation levels (erythropoietin), and increases bone mass through calcium and phosphorus regulation.
Homeostasis is an automated mechanism whereby concentrations of chemicals and fluids within the biological systems of an organism are stabilized. Kidneys contribute vastly to homeostasis, maintaining extracellular fluid volumes, acidity and alkalinity (pH), osmotic concentrations (concentration of solute molecules in a solution), and excreting potentially harmful products or excess molecules which can upset natural homeostasis.
Ureters
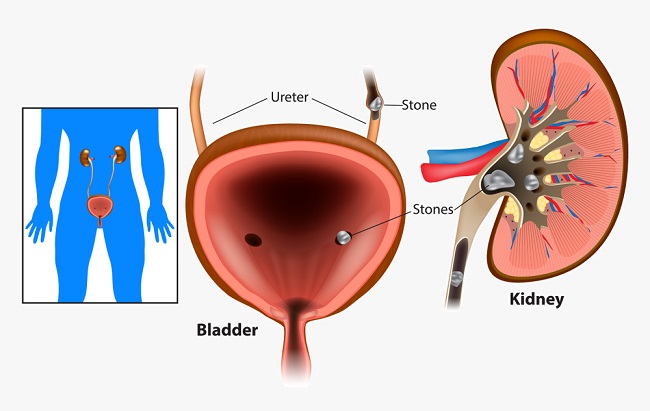
The urinary system includes two ureters which extend from kidney to bladder. Peristalsis and gravity bring urine along these narrow, hollow, thickly-layered tubes. Because the hollow areas are narrow, ureters can become blocked by debris such as salt crystals which have stuck together to create urinary stones. Complete blockage in one tube causes high pressures and urine buildup in its attached kidney and requires emergency surgery before permanent damage is done. Alternatively, reflux or the return of urine back into the ureters can cause infection and dangerously high pressures within the kidneys.
Bladder
The bladder is kept in place by a series of external ligaments. It’s main function is as a reservoir for urine. The bladder expands as it fills due to its thick layer of transitional epithelium. The cells of this layer can stretch and change shape, allowing the bladder to hold increasing amounts of urine. Two sphincter muscles stop urine from continually leaking out of the bladder. When this mechanism does not function properly incontinence is the result. The urinary nervous system provides the cues for bladder emptying and depends on signals sent from the stretch receptor cells inside the bladder wall. The image below shows the neural circuitry involved in urination.
Urethra
Urethra lengths differ in male and female urinary systems. The comparatively long male urethra that runs from the bottom of the bladder to the external urethral meatus of the penis is approximately 20 cm in length.
The urethra of the human female is only around 4 cm in length. This short length is the reason why women are more susceptible to urinary tract infections than men. The image below shows urinary catheterization in male and female subjects. Note the significantly longer length of the male catheter compared to that of the female.

The single urethra allows urine to pass outside the body once the brain has released the involuntary internal sphincter and the person in question has voluntarily released the external sphincter. No peristalsis occurs in the urethra – the passage of urine into the outside world is controlled by a combination of the pressure of the urine in the bladder, muscle tone, and gravity.
Urinary System Diseases
There are a huge number of urinary system diseases, from infections to cancer. Some of the most common are listed below.
Urolithiasis
Most kidney stones are small and simply pass through the urinary system without being noticed. Larger stones are most likely to become lodged in the narrow openings of either ureter. Low urine volumes and high salt concentrations in the urine contribute to stone formation. Stones are formed through the crystallization of salts. The presence of urinary system stones is referred to as urolithiasis.
Urinary Schistosomiasis
Parasitic flatworms called Schistosoma are the cause of urinary schistosomiasis or snail fever and are the cause of an extremely common tropical disease. Symptoms develop after the adults have laid eggs and include fever, shivering, cough, and muscle pain. Chronic forms present with symptoms much later on with the potential for ascites, blood in the urine, breathing problems, and overall weakness. It is also possible to experience seizures, paralysis, and changes in behavior and mental state in untreated chronic schistosomiasis.
Nephrotic Syndrome
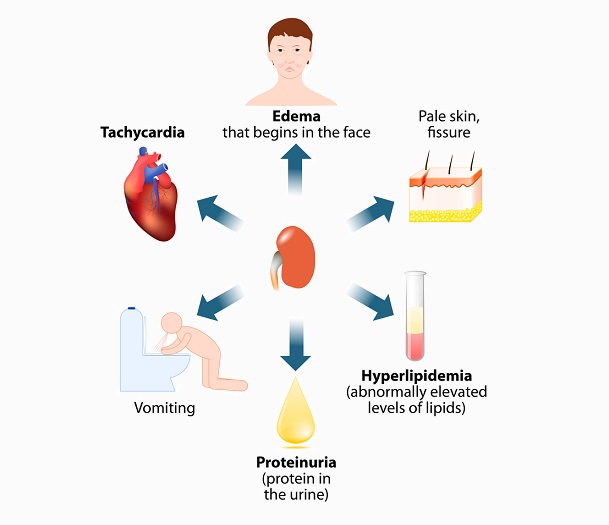
Nephrotic syndrome is not a disease in itself but the result of a wide range of kidney diseases. The main symptoms of nephrotic syndrome are fluid retention (edema) in the lower limbs and face, foam-like urine caused by high levels of proteins, fatigue, and loss of appetite. Fluid retention also causes significant weight gain. Any of the kidney diseases listed here have the potential to cause nephrotic syndrome if the filtering system of the nephrons becomes damaged and allows large molecules, primarily a protein found in the blood called albumin, to pass into the ultrafiltrate. Treatments of this syndrome need to manage the underlying cause(s) and not only the symptoms.
Urinary Tract Infections
Upper urinary tract infections (UTIs) involve symptoms such as high fever, shivering, vomiting, and pain in the loins. Lower urinary tract infections cause frequent, urgent or irregular urination, pain above the pubis (suprapubic pain), and sometimes traces of blood in the urine. The main cause of both types of infection is the E. coli bacteria, transferred into the urinary tract via the anus.
Chronic Kidney Disease and Chronic Renal Failure
Chronic kidney disease (CKD) can be inherited, as in autosomal dominant polycystic kidney disease (ADPKD), be the long-term result of acute kidney infection or trauma, or occur through a process in which damage to the urinary system takes place over many years. Approximately 70% of patients with CKD are diabetics, hypertension patients or patients presenting with atherosclerosis. These three diseases are often comorbid. Over time, nephron function is reduced through high levels of larger molecules passing through the nephrons, hormonal imbalances, or nervous system degeneration. All of these scenarios are caused by a low oxygen supply or hypoxia.
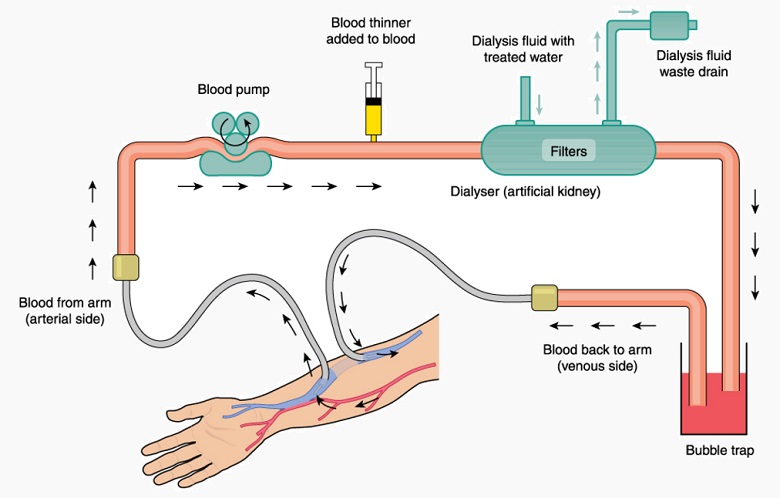
When both kidneys are no longer able to function, chronic renal failure is the result. In these cases, dialysis via the peritoneum of the abdominal cavity or via the circulatory system (hemodialysis) must take over all of the kidneys’ roles.
Acute Kidney Injury
When long-term illnesses are not the cause of kidney degeneration, trauma or short-term illness can cause acute kidney injury (AKI), otherwise known as acute renal failure. Nephrons are damaged by a sudden lowering of the blood supply due to hypovolemia. This can even be the result of excessive vomiting or long-term diarrhea. Symptoms include low amounts of urine, swelling in the lower limbs, fatigue, trouble breathing, confusion, nausea and chest pain. If left untreated, AKI can lead to convulsions and death. Immediate treatment is mandatory, where either injury or illness (or both) recovery allows the blood volume to be restored. Short-term hemodialysis is sometimes necessary to take over the role of the kidneys until the patient has stabilized.
Diabetic Nephropathy
When untreated or badly managed, diabetes causes high levels of glucose in the blood, giving it a syrupy consistency. Over time, high glucose levels damage the nephrons and they begin to leak proteins into the urine. Diabetic African Americans and Hispanic populations are particularly susceptible to renal disease caused by type 2 or type 1 diabetes.
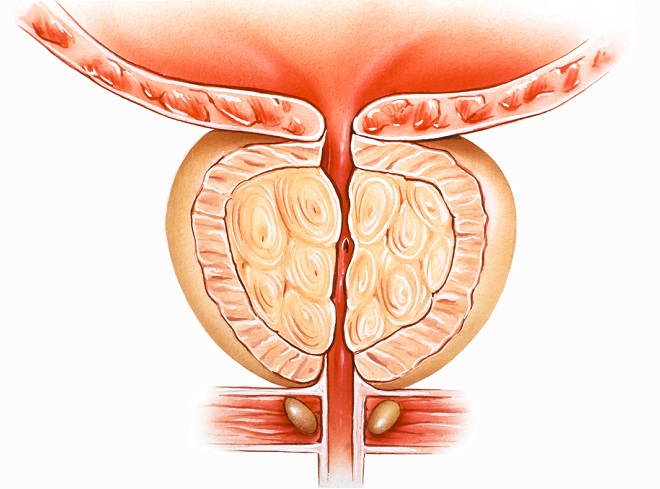
Benign Prostatic Hyperplasia
The non-malignant form of prostate enlargement affects elderly males. Urologists agree that all men from the age of sixty have some degree of prostate enlargement. While this is not a life-threatening disease, the enlarged prostate can push against the urethra and narrow it, causing frequent urination, a weak urine stream, and incontinence. Treatment includes muscle relaxant or prostate-shrinking drugs or prostate removal in a surgical procedure.
Quiz