Definition
The paired pulmonary artery that runs from the right ventricle into the right and left lung delivers deoxygenated blood within the pulmonary circulation system. The single pulmonary trunk that lies behind the pulmonary valve splits into right and left pulmonary arteries that are elastic when healthy. When this elasticity is lost, pulmonary arterial hypertension can occur.
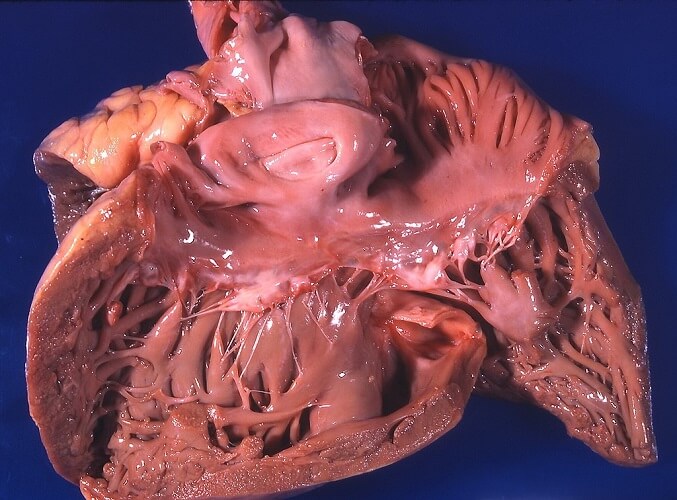
Pulmonary Artery Anatomy
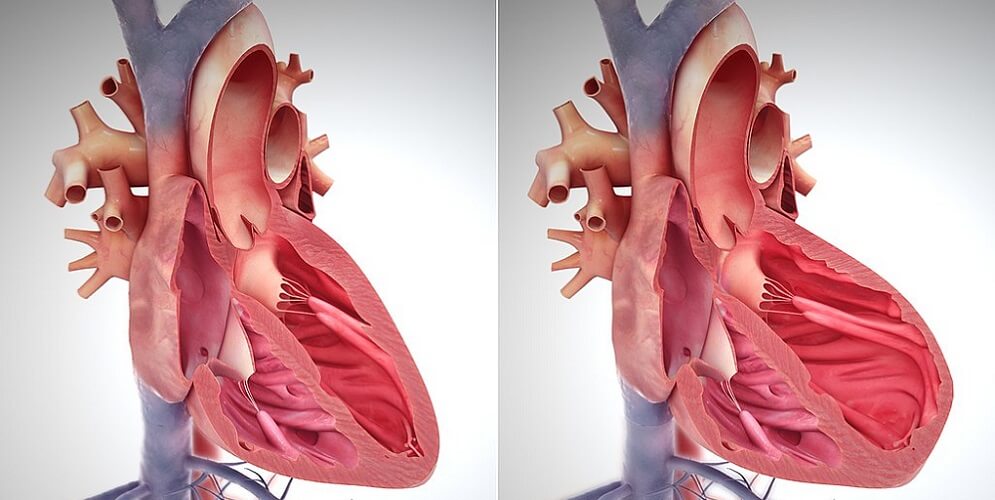
The main pulmonary artery exits the heart above the pulmonary valve of the right ventricle. This pulmonary trunk has a length of approximately five centimeters and a width of around three centimeters. It lies to the left of the aorta.
Just before the aortic arch the pulmonary trunk branches into a shorter left and longer right main pulmonary artery. The reason for this difference in length is due to the position of the heart that sits a little to the left of the midline.
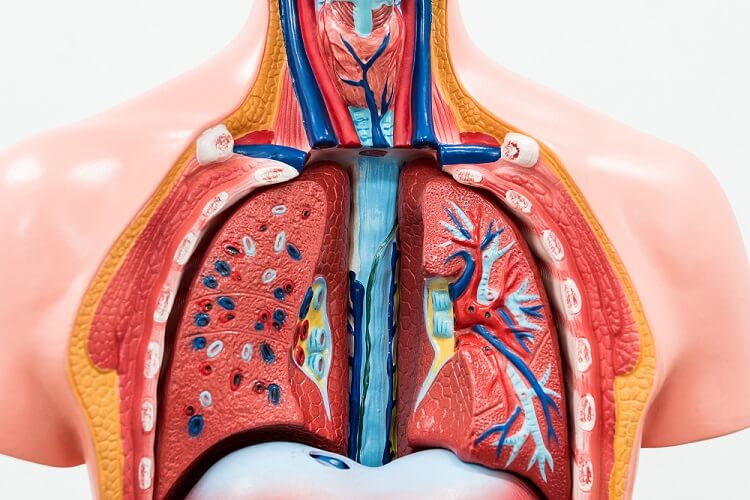
The left pulmonary artery (LPA) branches at a location known as the transthoracic plane of Ludwig. This is an artificial horizontal line used to divide the thoracic cavity into an upper and lower region. The LPA arches slightly behind and over the left main bronchus of the lung and enters at the left lung hilum. A hilum is an area where blood vessels and nerves converge to enter an organ – in this case the lung. In 97% of the population, the left pulmonary hilum is higher than the right.
The left main pulmonary artery then divides into branches. The branches that send deoxygenated blood to the top of the left lung are called left upper lobe (LUL) branches; those that send blood to the left lower lobe (LLL) are left lower lobe branches. The left lung lobes are further divided into segments that receive blood from even smaller branches that originate at the left pulmonary artery.
The right main pulmonary artery runs close to the heart for most of its length, horizontal to and behind the ascending aorta and superior vena cava. The right lung has three lobes rather than two. It enters the lung at the right lung hilus and its first branch is the called the truncus anterior.
The truncus anterior sends blood to the right upper lobe (RUL). From this point, the main pulmonary artery becomes the interlobar pulmonary artery as it has now entered the lung. It has more branches than the left pulmonary artery as it must supply blood to three lobes – the upper, middle, and lower lobes. The right lung lobes are further divided into segments that receive blood from smaller branches that originate at the right pulmonary artery.
Pulmonary Artery and Vein
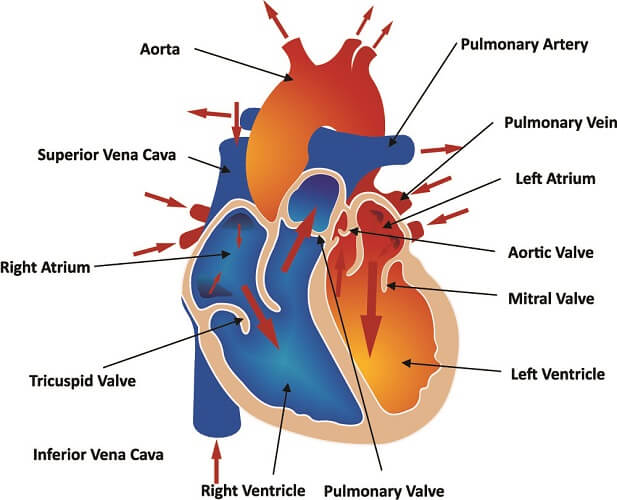
The pulmonary artery and pulmonary vein of the left and right lung have a different but extremely related function. Pulmonary artery function is to transport deoxygenated blood from the right side of the heart to the lungs. The pulmonary vein returns newly-oxygenated blood to the left side of the heart.
Just as in the cardiovascular system, the arterial and venous systems are connected through a network of smaller arterioles, venules, and capillaries. Capillaries surround the lung alveoli that provide a huge surface area for gaseous exchange – it is here that alveolar diffusion takes place.

Pulmonary Artery Pressure
Normal pulmonary artery pressure (PAP) is much lower than systemic blood pressure. Systemic pressure must pump blood throughout the body and normal values are approximately 120/80 mm Hg.
In the pulmonary circulation, normal arterial pressure is around 25/10 mm Hg. High pressures are unnecessary as the lungs lie so close to the heart. Furthermore, the alveoli are delicate and can be damaged when pressure is too high.
Pulmonary artery pressure rises very slightly as our oxygen saturation drops during sleep. This higher pressure usually remains within the normal range. In a small percentage of people with chronic obstructive pulmonary disease (COPD), lower levels of oxygen do not tell the brain to dilate the arteries. This leads to hypoxia (low tissue oxygen levels). Over time, the pulmonary artery walls change and are even less likely to respond to low-oxygen signals. Constantly constricted pulmonary arteries stop the right-hand side of the heart from emptying. This is the start phase of right-sided heart failure.
Sleep-disordered breathing also seems to have an abnormal relationship with PAP, although it is more likely that these people already suffer from pulmonary hypertension. This disease will be looked at in the following section.
Pulmonary Artery Disease
Pulmonary artery disease is a subcategory of pulmonary vascular disease (PVD). PVD affects the veins and arteries that connect the lungs and heart. The primary symptom of PVD is shortness of breath due to an inefficient oxygen supply.
When the pulmonary circulation must constantly deal with higher-than-normal pressures a diagnosis of pulmonary hypertension is likely. This diagnosis is given when average (mean) pulmonary arterial pressures are 25 mm Hg or higher.
There are three main causes of pulmonary hypertension:
- Pulmonary arterial hypertension
- Pulmonary venous hypertension
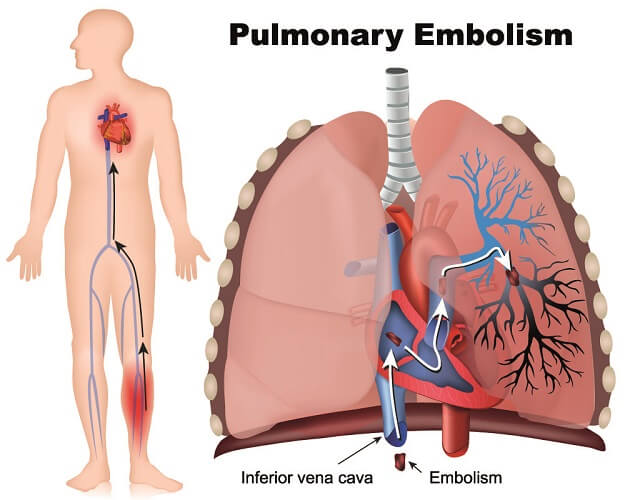
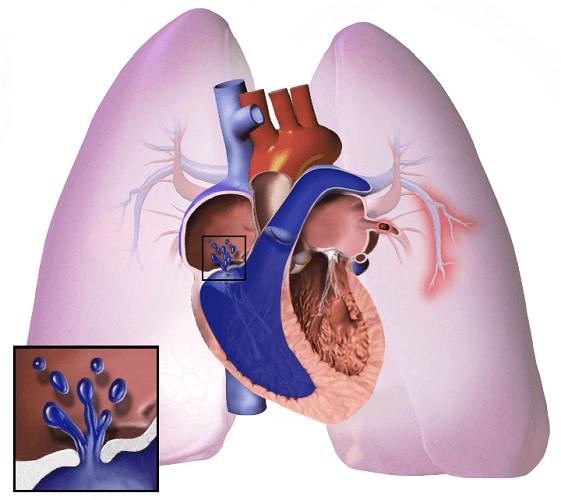
- Pulmonary embolism
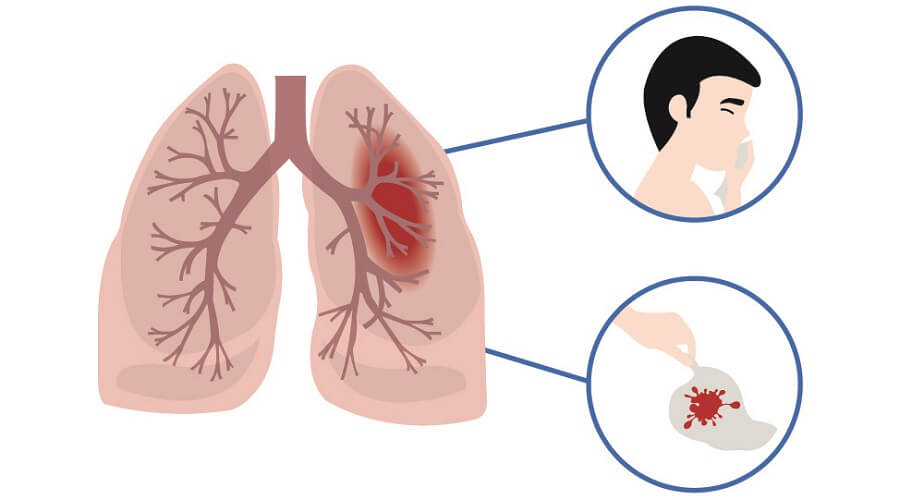
Embolisms are blood clots, air bubbles, pieces of arterial plaque, or fat droplets that cause blockages in the circulatory system. Once these become trapped in a smaller blood vessel, any tissue after that point can become oxygen-starved and die off. When this happens in the lungs and no immediate treatment is given, the results can be catastrophic.
Pulmonary venous hypertension is the result of congestive heart failure or problems with the mitral valve that lies between the left atrium and left ventricle. In the latter case, blood flows back from the ventricle into the atrium – a mechanism known as regurgitation. This stops the pulmonary veins from emptying blood into the heart and so increases pulmonary vein pressure.
Pulmonary arterial hypertension (PAH) is caused by medications, toxins, genetic mutations, connective tissue disease, infection, liver disease, blood disorders, damaged lung blood vessels, and various types of heart disease.
Pulmonary hypertension can take years to develop. Symptoms progressively get worse and include:
- Shortness of breath
- A bluish tint to lips and skin
- Coughing up blood
- Fatigue and dizziness
- Chest pain
- Swollen ankles, legs, and abdomen
- Rapid heart rate or palpitations

Pulmonary hypertension risk factors are:
- Age
- Family history of PAH
- Obesity
- Blood clotting problems
- Genetic disorders
- Medication
- Smoking
- Asbestos exposure
- Living at high altitudes
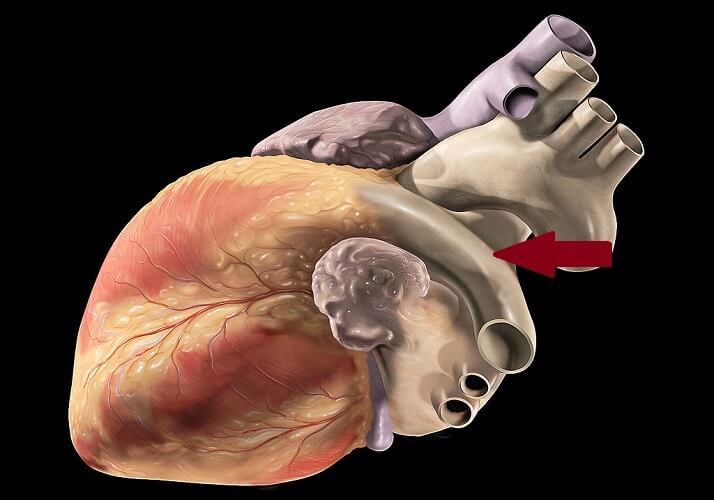
When pulmonary artery pressure is high, the effects spread to the heart. Cor pulmonale describes a large right ventricle; this part of the heart must work very hard to force blood through stiff and damaged pulmonary arteries. Reduced blood flow in the lungs also means that blood can develop small clots. These can block smaller vessels of either lung – a pulmonary embolism.
The heart is continuously responding to chemical and pressure messages via the autonomic nervous system. Pulmonary artery disease triggers compensation mechanisms such as a rapid heart rate. This heart rate can become irregular – arrhythmia – over time; this leads to symptoms such as dizziness and fainting.
Higher pressure in the blood vessels of the lungs also damages the delicate capillaries and alveoli. Alveolar diffusion becomes compromised and oxygen supply to the heart is much less efficient. Damage to the lung capillaries means that someone with chronic pulmonary hypertension may often cough up blood.