Definition
The neuromuscular junction (NMJ) is the connecting area between the end of a motor neuron and a muscle. It is here that the acetylcholine-dependent nerve impulse (action potential) is transmitted from neuron to muscle – hence the term neuromuscular. Sometimes referred to as the motor endplate, the NMJ is composed of a presynaptic and postsynaptic membrane and a gap between the two called the synaptic cleft. Many drugs and several disorders can affect this site.
What is a Neuromuscular Junction?
The neuromuscular junction is composed of three parts:
- Presynaptic motor nerve terminal
- Synaptic cleft or junctional cleft
- Postsynaptic muscle fiber
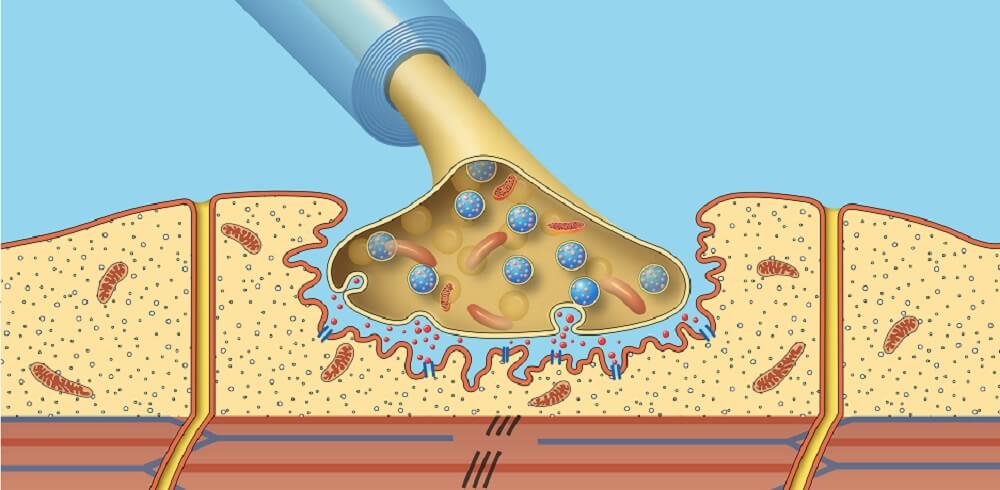
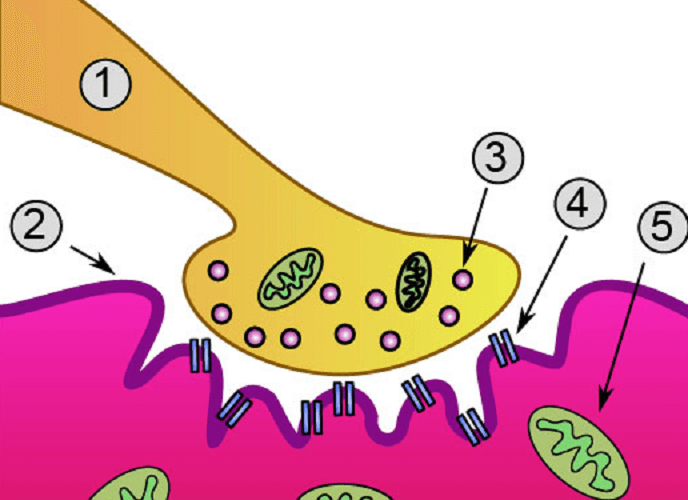
To better understand what a neuromuscular junction is, we should first look at the structure of the motor neuron terminal (1, 3), the synaptic cleft (2), and muscle membrane (4, 5). The labeled neuromuscular junction below shows these main components.
Motor Neuron
There are two main locations for motor neurons – upper and lower. These nerves allow voluntary and involuntary muscle movement throughout the body. They also control glands. Upper motor neurons begin in the cerebral cortex of the brain and travel to either the brainstem or the spinal cord. Lower motor neurons start in the spinal cord and it is these that directly connect to the muscles and glands. The neuromuscular junction, therefore, is only found in lower motoneurons. Even the cranial nerves which innervate the muscles of the skull and face synapse with the cell bodies of lower motor neurons in an area called the motor nucleus.
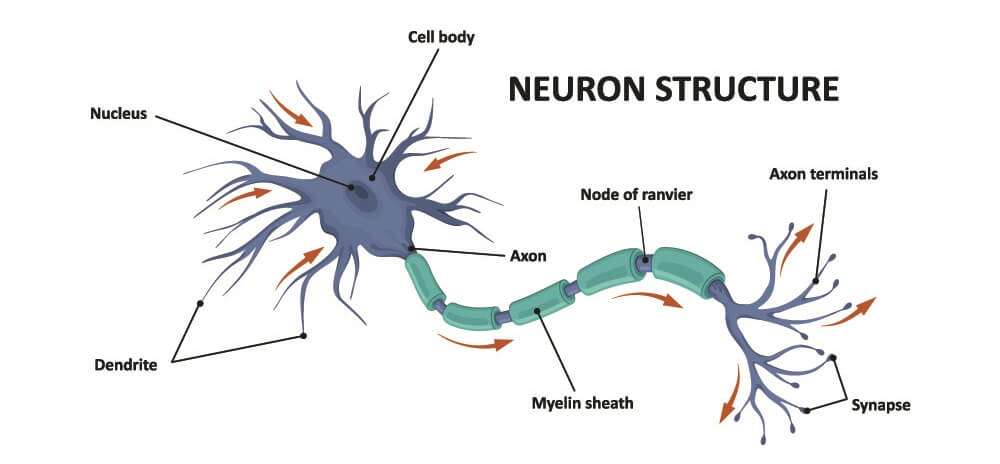
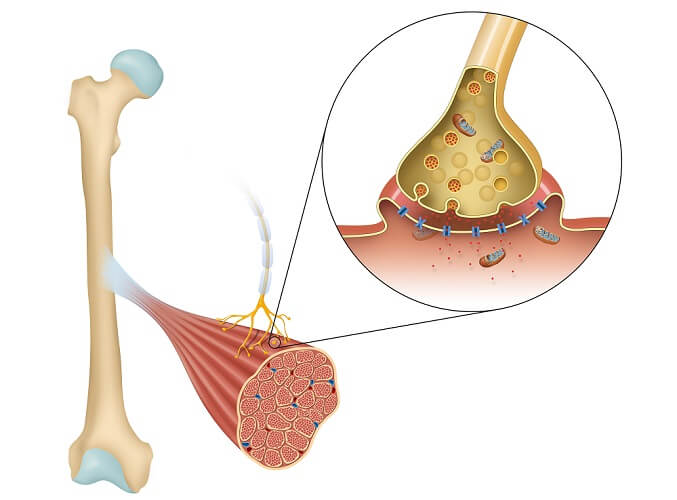
The important part of the motoneuron in terms of the NMJ is the terminal end. Where the terminal end begins, the insulating myelin layer that covers the axon is lost. At this point, the nerve branches into one to two hundred nerve terminals. Nerve terminals can also be referred to as boutons or terminal buttons. Each of these endings lies close to the membrane of a muscle. A small gap lies between the bouton and the muscle membrane called the synapse. This is why the terminal of a nerve is called the presynaptic terminal.
At each terminal, the membrane of the nerve becomes thick. This allows for the formation of synaptic vesicles filled with neurotransmitter molecules. Where the bouton membrane is thick is referred to as its active zone. The active zone contains special proteins, voltage-gated calcium channels, and potassium channels. It also contains a variety of cell organelles including mitochondria and endoplasmic reticulum. Many mitochondria mean there is enough energy for acetylcholine synthesis.
Junctional Cleft
Between bouton and muscle exists is a gap of around fifty nanometers (0.000005 cm). The neurotransmitter acetylcholine (ACh) released from vesicles in the active zone of the motor nerve terminal must cross this gap to cause an effect in the muscle. The synaptic cleft contains quantities of an enzyme called acetylcholinesterase (AChE). AChE helps to break down acetylcholine into acetic acid and choline much more quickly – it is a catalyst. Its role in the NMJ is to end a nerve impulse once it has reached the target muscle. Some pesticides and nerve agents inhibit the action of AChE. When this happens at the neuromuscular junction these products can cause muscle spasms or prevent nerve impulses from passing through, resulting in a neuromuscular blockade (paralysis).
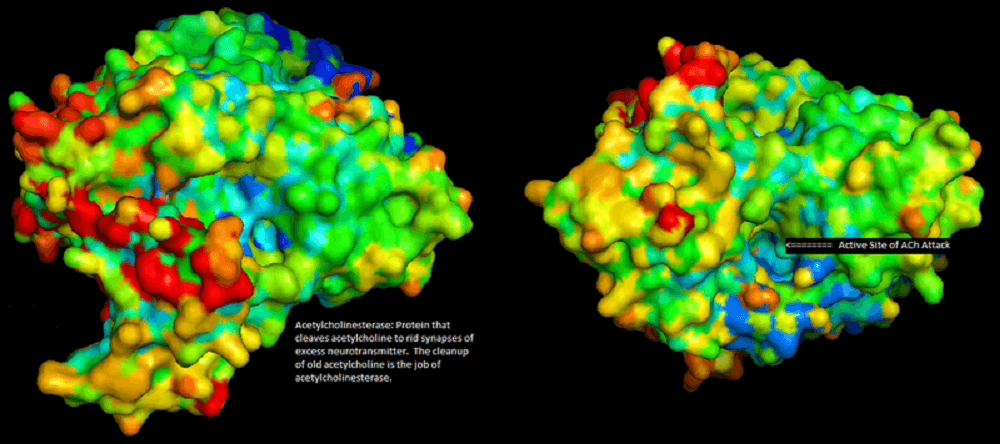
When acetylcholine is released from the terminal end, receptors on the target tissue accept it and signal that tissue to react. This reaction requires calcium ions (see neuromuscular junction steps). Without acetylcholinesterase, not only would the transmission rate be much slower, activation would continue for as long as acetylcholine remained inside the synaptic cleft. A muscle might fasciculate (spasm) for some time.
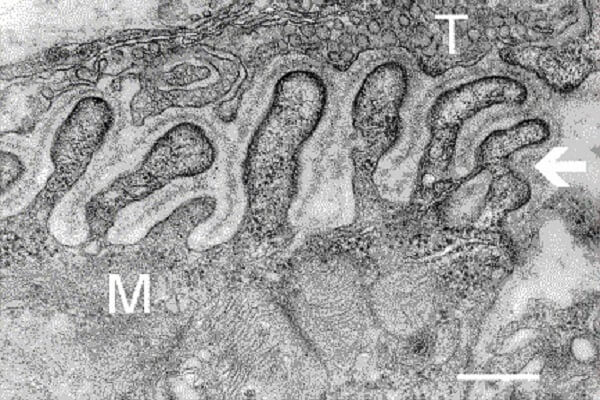
The junctional cleft between the terminal button and sarcolemma is part of the synaptic trough or gutter. The bouton does not sit slightly above the muscle membrane as the majority of images show but molds loosely around the folds of the postsynaptic membrane. Even so, the synaptic gap still exists. There is no direct contact between the presynaptic and postsynaptic neuromuscular junction parts. In the electron microscope neuromuscular junction diagram below, where T indicates the motor neuron terminal and M the muscle fiber, the postsynaptic folds (arrow) are easy to see.
Postsynaptic Membrane
The postsynaptic part of the motor endplate is positioned on the receiving end of the synaptic cleft. As already mentioned, this membrane is folded. These folds are called subneural clefts and are necessary to increase the surface area of the synapse. The more opportunity there is for acetylcholine to cross the cleft and fit into postsynaptic receptors, the better the transmission quality.
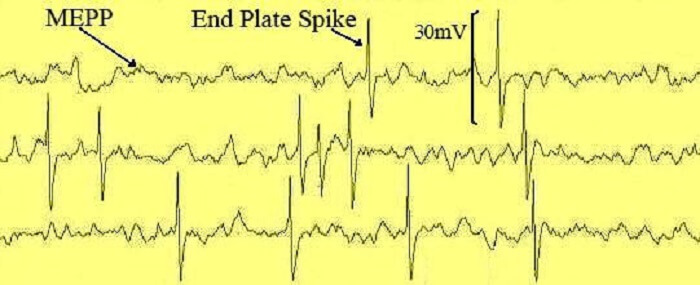
The power that is caused by changes in membrane voltage by the acceptance of ACh in the motor endplate receptors can depolarize a muscle fiber and cause it to contract. Between +50 and +75 millivolts are required. This power surge is called the end plate potential (EPP). A single vesicle containing ACh only produces a potential of approximately 0.4mV – these are called miniature end plate potentials (MEPPs) and are depticted in the image above. Only higher-volume release from large numbers of vesicles can produce the voltage changes that forward a nerve impulse. When enough is released to produce at least +50 mV, muscle contraction can occur. This mechanism stops contraction from taking place when only small quantities of ACh are available.
During general anesthetic where synthetic curare is used, this drug replaces acetylcholine in the motor endplate receptors. The muscles are then unable to contract. This is why such drugs are sometimes referred to as skeletal muscle relaxants. They do not affect heart muscle contraction as cardiac muscle implements a different system.
There are two main types of ACh receptors – nicotinic and muscarinic. The latter is found predominantly in the autonomic nervous system and helps glands to secrete chemicals. Most textbooks will tell you that only nicotinic receptors are found in the NMJ; this is not strictly true. Muscarinic receptors are found on the presynaptic membrane and help regulate acetylcholine release. The postsynaptic membrane of the motor endplate, however, is composed of nicotinic and not muscarinic receptors.

Neuromuscular junction nicotinic receptors are found in an area called the perijunctional zone. This zone also contains many sodium channels and is extremely close to the motor nerve ending. Different variants of nicotinic acetylcholine receptors (nAChRs) and sodium channels are found at different life stages and can also become damaged. One example of a congenital motor plate anomaly is Eaton Lambert syndrome that presents with symptoms such as muscle weakness.
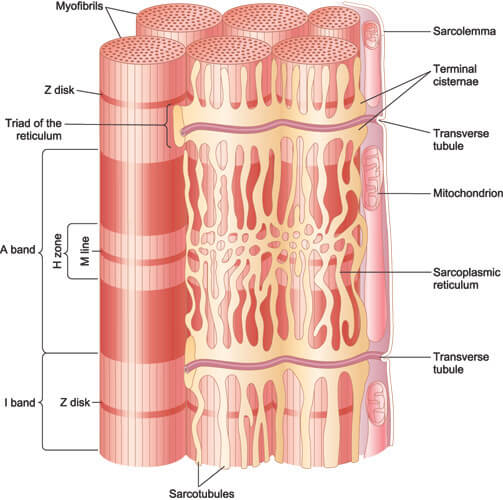
Muscle fibers are bundled together within a membrane called a sarcolemma or myolemma. The sarcolemma contains all manner of channels as well as the all-important nicotinic receptors of the NMJ. When the nAChR are filled with neurotransmitter, sodium ions rush into the sodium channels of the sarcolemma. It is these ions that cause the voltage changes along the membrane that define an action potential. This action potential moves into the underlying muscle fiber and stimulates calcium ion channels in the sarcoplasmic reticulum. Calcium ions can then cause contraction of the actin and myosin proteins inside the muscle cell.
Neuromuscular Junction Steps
Events at the neuromuscular junction follow these stages:
- The motor nerve forwards an impulse along its axon until it reaches the axon’s end.
- This action potential opens calcium ion channels at the end of the axon.
- Calcium ions flow into the motor nerve cell.
- Intracellular calcium sends vesicles to the edge of the presynaptic membrane.
- Vesicles fuse with the membrane and release ACh into the synaptic cleft.
- ACh molecules move through the cleft toward the postsynaptic membrane.
- Postsynaptic nicotinic ACh receptors attach to ACh.
- Once attached, sodium ion channels in the postsynaptic membrane open.
- Increasing levels of bonded receptors produce enough voltage for an EPP.
- The impulse that moves into the muscle fiber is released and contraction occurs.
Neuromuscular Junction Neurotransmitters
What neurotransmitter is released at the neuromuscular junction? Only one – acetylcholine. Acetylcholine levels are regulated by quantity, the effects of muscarinic AChRs in the presynaptic membrane, and the presence and quantity of acetylcholinesterase in the synaptic cleft.
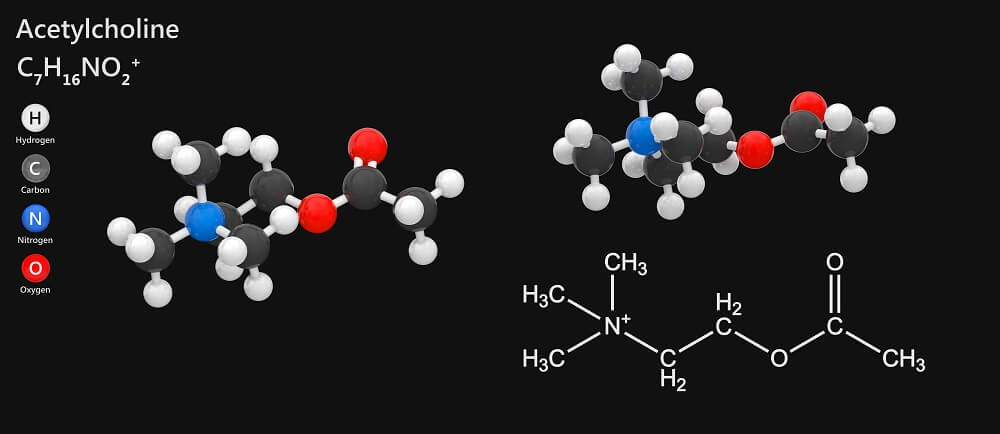
While synapses between nerve cells can depend on a range of neurotransmitters such as adrenaline and dopamine, in a motor end plate the transmitter is always ACh.
Neuromuscular Junction Disorders
It is most commonly autoimmune disorders and genetic mutations that cause problems with NMJ transmission. We have already looked at Lambert-Eaton syndrome. Another autoimmune example is myasthenia gravis where the person makes antibodies – usually against AChRs. Less active receptors mean the muscles respond more slowly (if at all) and tire more quickly. The opposite effect is caused by Isaac’s syndrome where higher levels of ACh are released, resulting in twitching muscles that may or may not cramp but also tend to react less distinctly to the continuous action potentials.

Genetic forms of neuromuscular junction disorders span diseases such as muscular dystrophy and the group of congenital myasthenic syndromes. In muscular dystrophy, damage to muscle tissue also affects the postsynaptic membrane of the sarcolemma. Some syndromes affect the production and effect of acetylcholinesterase that also lead to NMJ malfunction. As neuromuscular junction function is to transmit a signal that causes a muscle to contract, any NMJ disorder will affect muscle movement, especially skeletal muscle movement.