Definition
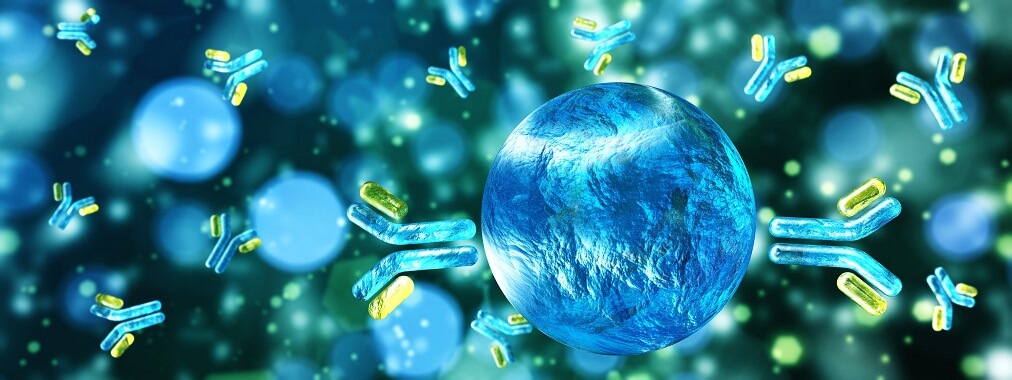
B cells or B lymphocytes are part of the adaptive immune response. Once activated, these white blood cells produce antibodies. B lymphocytes have further roles as antigen-presenting cells and cytokine secretors. This cell type is classified into four main groups: transitional, naïve, plasma, and memory B cells.
What are B Cells?
B cells are lymphocytes – a type of white blood cell. They are the result of multipotential cell differentiation in the bone marrow.
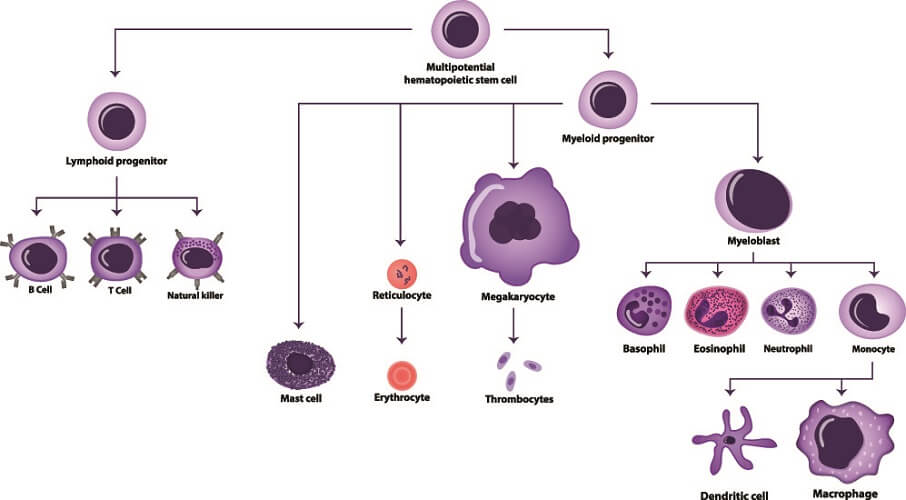
Every blood cell is derived from a single cell type – the pluripotent hematopoietic stem cell. This stem cell changes or differentiates into two forms within the bone marrow. One is the common myeloid progenitor that creates leukocytes, platelets, and red blood cells. The other is the common lymphoid progenitor. It is from the common lymphoid progenitor cell that B cells and T cells develop.
What Do B Cells Do?
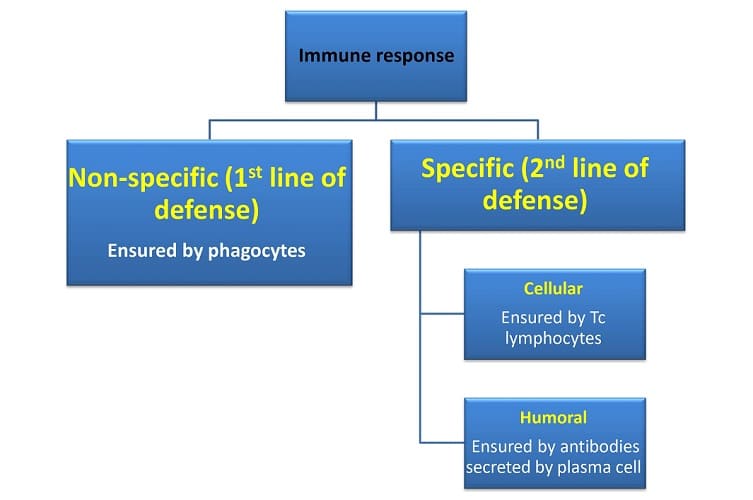
B cell function is threefold:
- Antigen presentation to other immune cells
- Cytokine secretion
- Antibody production
Before a B lymphocyte is activated, it does very little. In fact, as late as the 1960s most textbooks told us there was no B cell function. For an interesting history of lymphocyte research, have a quick read through this scientific paper.
Antigen-Presenting Cells
While the most important function of B cells is our humoral (antibody-driven) immunity, inactivated B lymphocytes also act as antigen-presenting cells (APCs).
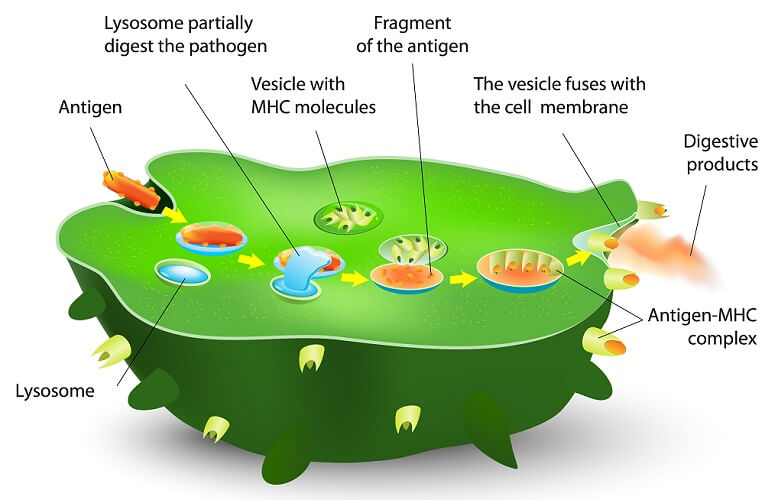
Antigen-presenting cells are found all over the body. They attach to an antigen (foreign particle) and process it, producing membrane markers that act as a warning (the antigen-MHC complex in the diagram above) that a T cell can understand.
B lymphocytes present these antigen-MHC complexes to T cell receptors, causing T cell activation.
Where the non-specific immune system (the innate immune system) is concerned, this reaction produces the opposite effect – T cell inactivation. This indicates that B lymphocytes also help prevent autoimmune reactions.
Cytokine Secretion
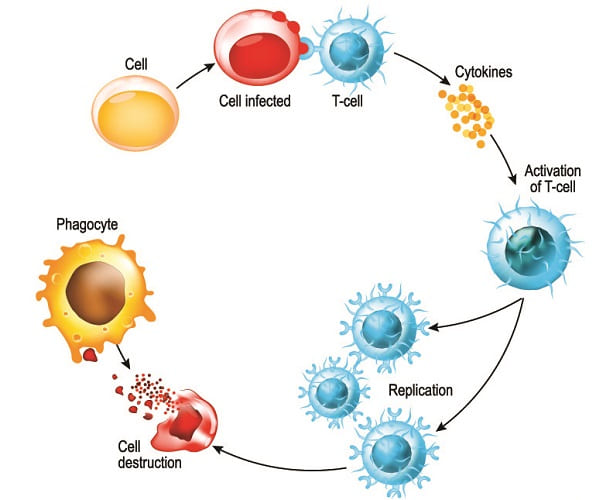
Cyto (Greek for cell) and kinos (Greek for movement) describes the action of cytokines – they cause cell movement. Cytokines are signalling molecules and essential for cell-to-cell communication.
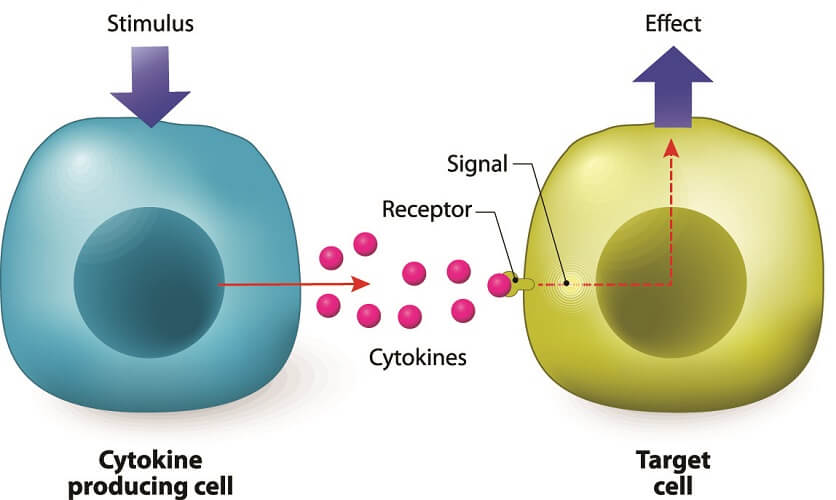
When B lymphocytes release cytokines, they invite white blood cells in the form of phagocytes to the areas where B-cell antibodies have attached to antigens.
Antibody Production
The primary function of B cells is antibody production. To understand this phenomenon, it is important to have some knowledge of the humoral immunity process.

Humoral immunity begins in the B lymphocyte. While still in the bone marrow, a B cell develops special membrane receptors called B-cell receptors (BCRs). These proteins are the equivalent of locks that fit antigen keys. B lymphocytes then relocate to the lymphoid organs. Once there, they are called naïve B cells.
When a naïve B lymphocyte comes into contact with an antigen that fits its receptors, it binds to it and brings it inside its membrane (endocytosis) for processing. This processing is important as it leads to the formation of antigen-MHC complexes that T cells can recognize.
Contact with an antigen does not cause B cell activation. When a T cell binds to the antigen-MHC complex it releases cytokines. These T-cell cytokines activate the B lymphocyte.
Activation means that the B lymphocyte divides to form one of two types of daughter cells; activated plasma cells or inactive memory cells.
Memory cells have longer lifespans and will recognize the same antigen should it attack at a later date. Plasma cells respond immediately through the release of antibodies. Tiny antibodies circulate throughout the blood, ready to attach to their specific antigen type.
How Do Antibodies Work?
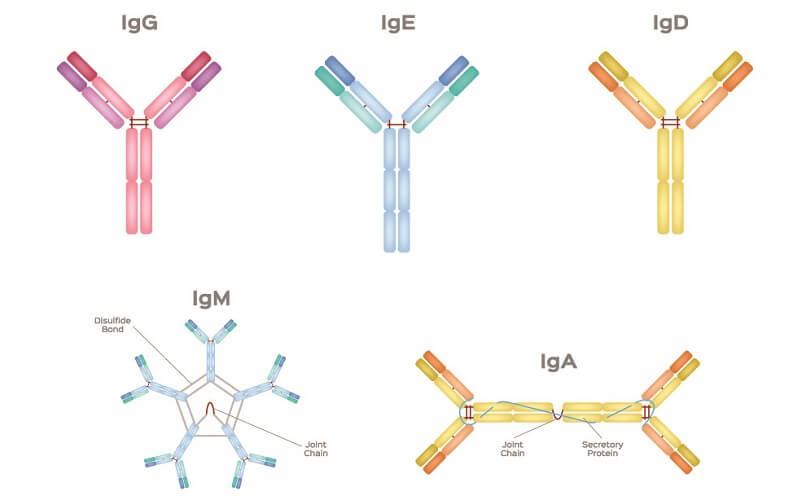
Antibodies or immunoglobulins are split into five classes:
- IgM: first response; causes many types of antigens to clump together
- IgA: protects against mucous membrane pathogens
- IgD: receptor function – signals B cell activation, usually co-expressed with IgM
- IgG: the most common human immunoglobulin – marks a broad range of pathogens for disposal
- IgE: binds to mast cells and basophils and causes histamine release – linked to allergies
An antibody can inactivate an antigen using three different processes.
The first is complement fixation. In complement fixation, the antibody binds to a foreign particle and breaks it down. This process also attracts other white blood cells through chemotaxis (chemical – cytokine – messaging). Antigens are destroyed through opsonization (antibodies mark them so other cells can recognize and destroy them).
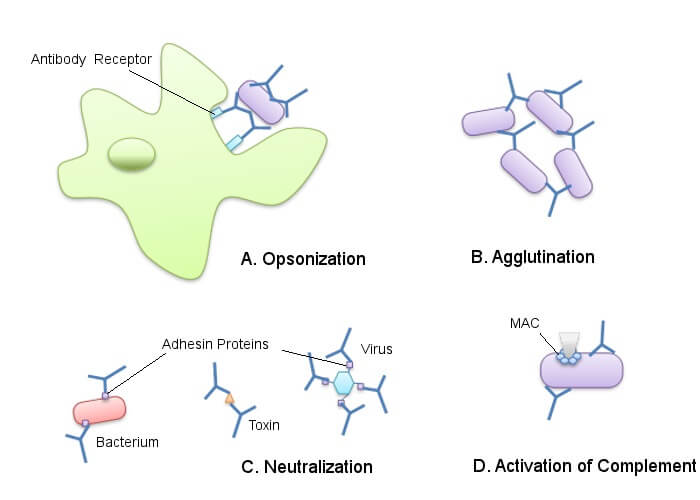
Another way in which antibodies attack antigens is through neutralization. When an antibody binds to an antigen, it prevents that antigen from releasing toxins.
The final method is agglutination where antibodies cause the foreign particles to stick together. Once clumped into a group it is easier for phagocytes (digesting cells) to remove them. This is how IgM antibodies work.
B Cell Types
There are four main B cell types: transitional, naïve, plasma, and memory cells.
Transitional B Cells
A transitional B cell is the link between immature B lymphocytes in the bone marrow and mature B cells in lymphoid organs. These cells have differentiated into B lymphocytes from common myeloid progenitor cells in the bone marrow; however, they are not yet mature.
The maturation process occurs in the lymphoid organs. Between production in the bone marrow and maturation (not activation) in the lymphoid organs, a B cell is referred to as a transitional B cell.
Very few immature B cells live long enough to become mature. It is thought (but not yet proven) that too many transitional B cells can trigger autoimmune disorders such as lupus erythematosus and rheumatoid arthritis.

Naïve B Cells
Naïve B cells are located in the secondary lymphoid organs. They are mature but not yet activated. Naive B lymphocytes can differentiate into plasma or memory B cells.
A further role pairs naïve B cells with naïve T cells to stop the latter from proliferating. This action has led to a new B cell subcategory – Breg cells (regulatory B cells). We are only just beginning to learn about them. As their full name suggests, Bregs limit the humoral immunological response by lessening T-cell responses.
Plasma Cells
Plasma cells or effector B cells are the cloned daughter cells of activated naive B cells. Plasma cells produce antibodies but this is a rather slow response to antigen detection.
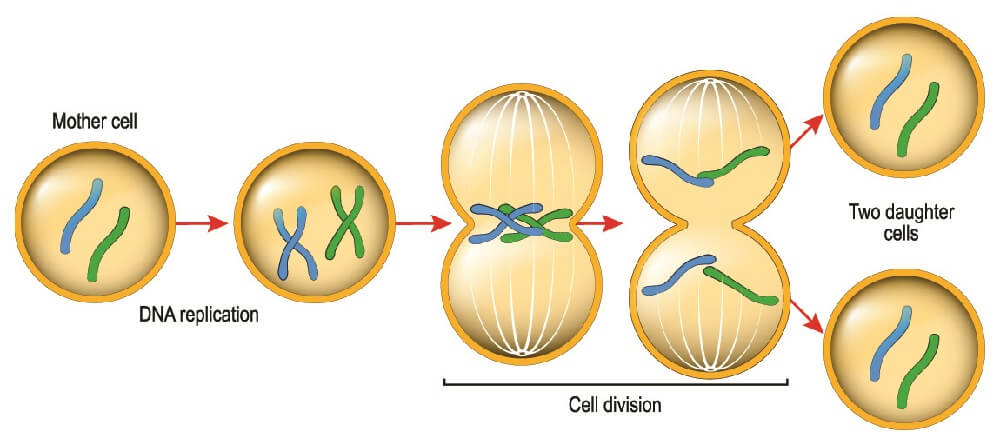
Two processes are necessary to produce plasma cells. First, a naïve B cell must present an antigen to a helper T cell. The now-activated T cell must, in return, switch on the B cell. This double authentication process turns a naïve B cell into an activated B cell. Only an activated naive B cell can divide to produce plasma cells or memory cells.
We do not always need T helper cells to initiate a generalized humoral response. B cells can activate themselves through a process called T cell-independent antigen stimulation. They divide to form daughter-cell clones that can only secrete IgM antibodies.
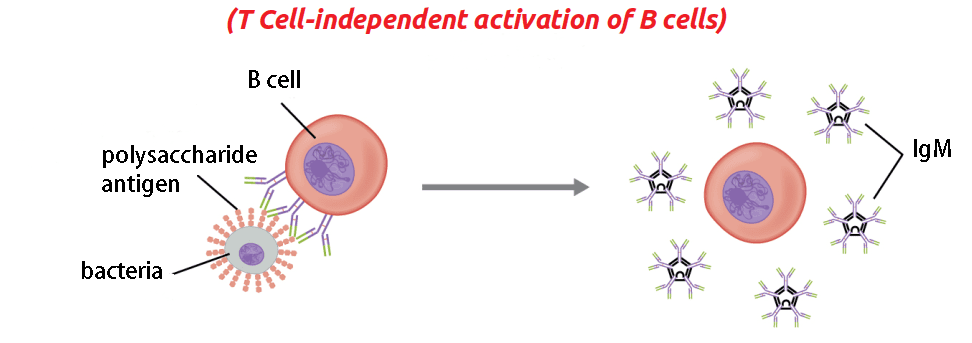
Plasma cells secrete antibodies that attach to the type of antigen that was first processed by the naïve B cell. T cell-independent activation only produces IgM immunoglobulins. A plasma cell cannot secrete more than one type of antibody. Plasma cells move around the body according to the distribution of cytokines, secreting antibodies closer to the source of the attack.
Memory Cells
A low percentage of plasma cells differentiate into memory cells. Memory B cells have much longer lifespans (years) than plasma cells (days to months). We do not yet know what causes a B cell to differentiate into either form.
Memory cells spread around the body. Just like the plasma cell, they have a specific affinity for one type of antigen. Their longer life means that, when plasma cells have finished their task and an antigen is defeated, a second attack at a later date will trigger a much quicker response.
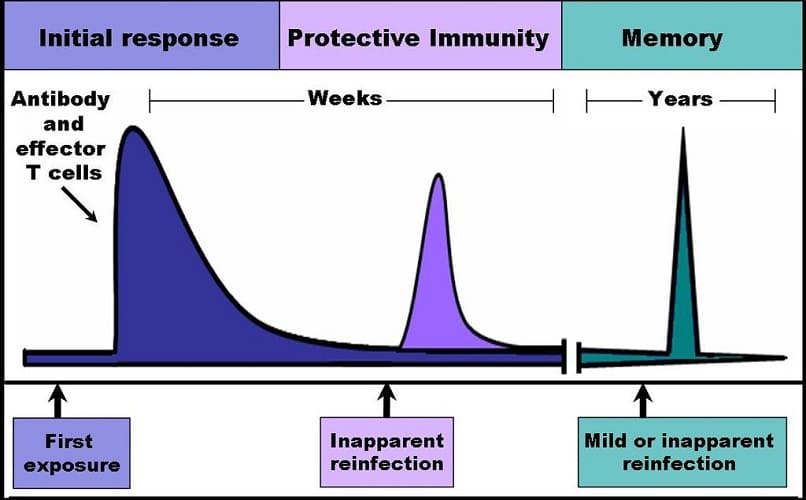
A second exposure to the same antigen makes memory B lymphocytes divide to form plasma cells. This occurs at a rapid rate and is called the secondary immune response.
B1 and B2 Cells
The B lymphocytes discussed in this article are B2 cells derived from pluripotent hematopoeitic stem cells in the bone marrow.
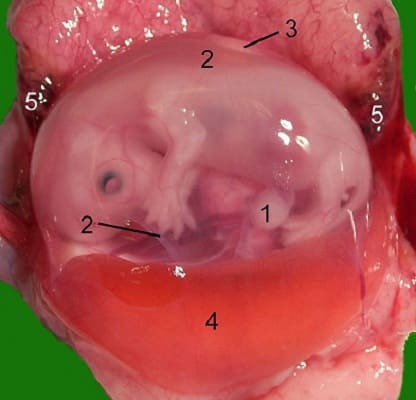
Recent research has found another, much smaller group of immune cells – B1 cells. These develop in the yolk sac of an embryo. Like B2 cells, they produce antibodies.
B Cells vs T Cells
T cells and B cells contribute to our specific immunity and develop from the same progenitor stem cell. However, they have many differences.
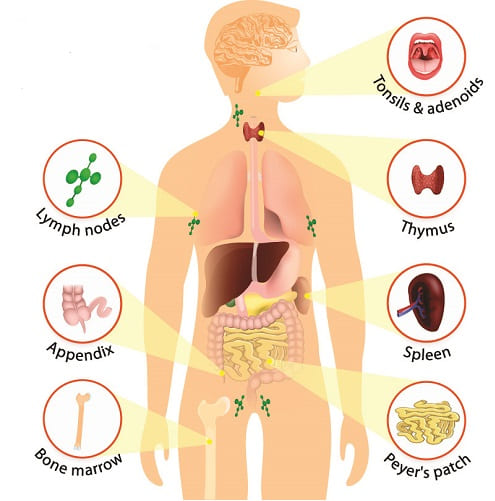
- B lymphocytes differentiate inside the bone marrow; T lymphocytes differentiate in the thymus. These are the primary lymphoid organs.
- T lymphocytes mature in secondary lymphoid organs such as the lymph nodes, spleen, tonsils, and appendix; B lymphocytes mature in the bone marrow.
- There are many more T cells than B cells. T cells make up around 80% of all circulating lymphocytes.
- T lymphocytes tend to be more diffusely distributed in the lymph nodes; B lymphocytes collect in tighter groups.
- B cells are the foundation of humoral immunity. Humoral immunity is antibody-mediated immunity; T cells are part of our cell-mediated immunity and activate other immune cells.
- T cells live much longer
- T cells cannot recognize an antigen without it being presented by an APC. The B cell does not always need a T cell to activate.
- When activated, B lymphocytes become antibody-secreting plasma cells or memory cells; T lymphocytes become one of three types of effector T cells:
-
- Cytotoxic T cells: kill infected cells
- Helper T cells: activate naïve B lymphocytes
- Regulatory T cells: stop an immune response when danger has passed
B Cell Lymphoma
Blood cancers affect blood cell production. Lymphoma or cancer of the cells of the lymphatic system most often affects B lymphocyte development and production.
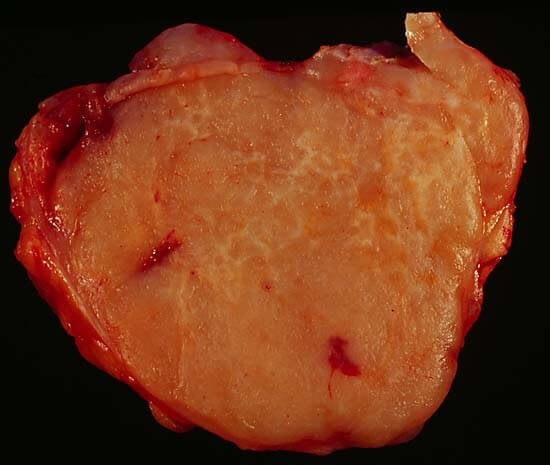
B cell non-Hodgkin lymphoma (NHL) makes up 80% of all non-Hodgkin cases. This cancer type is further sub-categorized into:
- Diffuse Large B-Cell Lymphoma (DLBCL): usually affects elderly populations. Fast growing. High cure rate.
- Follicular Lymphoma: usually affects elderly populations. Slow growing.
- Mantle Cell Lymphoma (MCL): usually affects elderly males. Fast growing and difficult to treat.
- Marginal Zone Lymphoma: usually affects elderly populations. Slow growing.
- Burkitt Lymphoma: usually affects male children. Fast growing. 50% cure rate.

B cell lymphoma treatment is usually limited to chemotherapy; it is impossible to irradiate the entire body.
DLBCL responds well to a mix of cytotoxic, steroid, and monoclonal antibody medications referred to as R-CHOP – a cocktail of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone.