Definition
Aldosterone (C21H28O5) is a mineralocorticoid hormone compound secreted by the adrenal gland cortex. It is part of the renin angiotensin aldosterone system or RAAS and is an integral part of the complex mechanisms that control water and electrolyte balance within the body. Its action affects sodium, potassium and water levels via the excretory and circulatory systems.
Aldosterone Function
The main function of aldosterone is to increase reabsorption within the latter portion of the distal tubule of the nephron and the collecting ducts. When working specifically at this location the hormone binds to mineralocorticoid receptors on the membrane of the distal tubule. Once bound, distal tubule membrane permeability increases. This makes it easier for potassium and sodium to pass through. Aldosterone also activates the mechanism of hydrogen ion secretion in the collecting ducts. This regulates the pH of the plasma and therefore is important in the acid-base balance. It is also understood that aldosterone has a further role in antidiuretic hormone (vasopressin or ADH) release from the pituitary gland whereby more water is reabsorbed into the body via the nephron. However, aldosterone only affects approximately 3% of total water reabsorption. It is therefore considered to be a fine-tuning mechanism which is more appropriate for small, regular changes in blood volumes rather than a saving measure in acute blood loss.
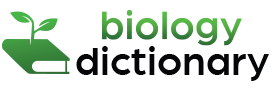
Aldosterone in the RAAS
The renin-angiotensin-aldosterone system or RAAS regulates blood pressure by way of a single pathway composed of various hormones. These hormones – renin, angiotensin, and aldosterone – work together to produce the enzymes responsible for vasoconstriction and regulate secretion and excretion in the kidneys. The RAAS works alongside the RAS or renin-angiotensin system to rapidly control blood pressure whenever required.
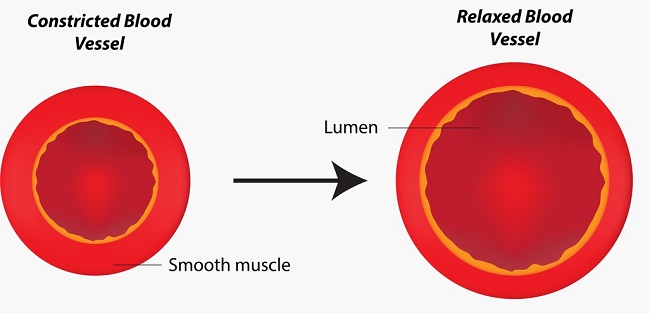
Renin or angiotensinogenase is an enzyme and a hormone produced by the kidney and is released when fluid levels in the body drop. Hypovolemia can be caused by dehydration, low water intake, long-term diarrhea or vomiting, blood loss, and systemic infections. The kidney requires a cue in order to release renin. This is given via the autonomic nervous system which responds to signals sent from specialized baroreceptor cells in the walls of the heart and major arteries. There are two types of baroreceptor – high and low pressure. They detect levels of stretch in the arterial, venous or myocardium. The former is located in the aortic arch and carotid artery. The latter in the pulmonary arteries, larger veins, and the myocardium. When the baroreceptors notice a drop in blood volume, renin is released. Renin transforms angiotensinogen to angiotensin I.
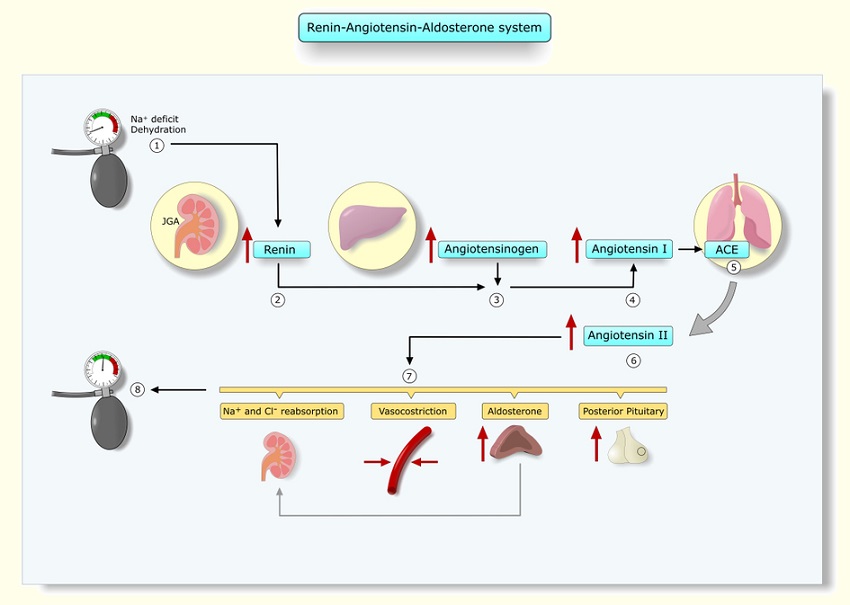
Angiotensinogen is a precursor protein and is manufactured in the liver. In the presence of renin, angiotensinogen is converted into angiotensin I, yet another precursor. In order to produce the final form, or angiotensin II, another enzyme produced by the lungs called angiotensin-converting-enzyme or ACE is necessary. The term ACE may be familiar, as ACE-inhibitors are popular drugs used to control chronic high blood pressure. By inhibiting this enzyme, blood vessels relax (see image below) and blood pressure does not reach dangerous levels. One ACE is released, angiotensin I is converted to angiotensin II.
Angiotensin II directly affects the blood vessel walls, constricting them and so raising blood pressure. It also ensures blood is available to the most important organs such as the heart, kidneys, and lungs. In the kidney, angiotensin II makes the arterioles that supply blood to each nephron constrict. The afferent or supply arteriole constricts a little; the efferent or exiting arteriole constricts much more. This causes the blood between these vessels to back up – a vital mechanism, as without continuous pressure the exchange of ions, water, and other molecules cannot take place within the nephron.
In addition to its effect on the musculature of the blood vessels, angiotensin also increases the reabsorption rate of sodium within the nephron. Increased concentrations of sodium attract increased concentrations of water. By reabsorbing more sodium into the blood, the nephrons automatically reabsorb more water, increasing the blood volume.
Angiotensin II also signals for the release of aldosterone from the adrenal cortex. Aldosterone increases the volume of water reabsorbed back into the circulatory system by enabling even more sodium reabsorption. In addition, both aldosterone and angiotensin II signals for the release of anti-diuretic hormone (ADH or vasopressin) from the posterior pituitary gland. As one of its names suggests, ADH is a vasopressor or vasoconstrictor. It also increases water reabsorption in the nephron as shown below.

Aldosterone vs ADH
While both aldosterone and antidiuretic hormone are hormones secreted in order to increase water volume within the body and both act at the distal convoluted tubules and collecting tubules of the nephron, this is where their similarities end.
ADH is a lipophobic and quick-acting peptide hormone. Aldosterone is a lipophilic, slightly slower working (but longer-lasting) steroid hormone, more specifically a corticosteroid hormone.
Aldosterone is both synthesized and released from the adrenal glands; the prohormone form of ADH is produced in the hypothalamus but released from the pituitary gland. Aldosterone also affects the movement of sodium molecules across the membrane of the nephron tubules by increasing their permeability, while ADH makes these membranes more permeable to water. This means that aldosterone increases osmotic pressure and ADH allows the water molecules to respond to this change.
The Baroreflex
When blood pressure levels rise, high-pressure receptors send signals to the brain which lowers the heart rate and dilates the blood vessels. When hypovolemia or sudden shunts of fluid from the circulatory system occur, such as in syncopal episodes, low-pressure receptors in the pulmonary arteries, large veins, and atrial and ventricular walls do the opposite. They send signals to the brain which result in an elevated heart rate and vasoconstriction. Both of these reactions are referred to as the baroreflex. Depending on the location of the baroreceptors, signals travel along the nerves and terminate at the medulla oblongata.
To lower blood pressure, the medulla oblongata activates parasympathetic nerves to reduce cardiac output. This occurs through a slower heart rate and less outspoken heart muscle contractions. At the same time, the medulla oblongata sends inhibitory signals to the sympathetic nerves which relax the blood vessel walls, causing vasodilation. This dilation means a larger space for the same amount of blood, leading to reduced blood pressure.
To increase blood pressure, the medulla activates sympathetic nerves which increase the heart rate and the strength of myocardium contractions which heightens cardiac output. Parasympathetic nerves are inhibited, through which the relaxing effect on the blood vessel walls is removed and the vessels constrict. This pushes a higher output of blood into a smaller space within the circulatory system and increases pressure within the blood vessels.
The Role of Adrenoceptors in Raising and Lowering Blood Pressure
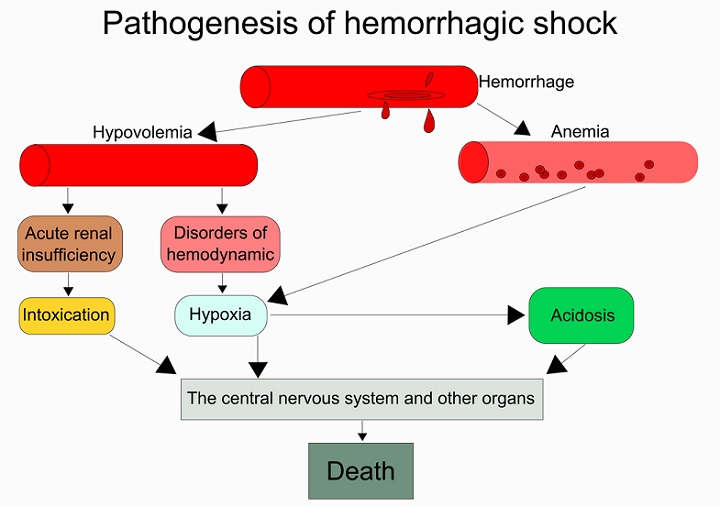
Other mechanisms are also at work when baroreceptors signal hypovolemia. These have a greater effect than the RAAS and are put into effect when pressures dip or rise well out of normal ranges. The steps that lead to hemorrhagic shock in cases of major blood loss, for example, are shown below. Note how low blood volumes lead to renal insufficiency due to the inability to maintain pressure in the glomerulus and so put an end to all filtration.
Adrenaline is released from a different region of the adrenal glands (the medulla), together with the neurotransmitter noradrenaline. These create alpha and beta effects to raise blood pressure. Both alpha and beta adrenoceptors are composed of two groups – 1 and 2. Alpha-1-adrenoreceptor agonists bind to alpha-1 receptors on peripheral blood vessels and cause their muscles to constrict, shunting the blood to more critical organs and systems. An agonist is a product which, when in contact with a receptor, initiates a chemical response. Alpha-2-adrenoreceptor agonists bind to alpha-2 receptors and inhibit norepinephrine (noradrenaline) release. Therefore, it has the opposite effect of alpha-1 function. Beta-1-adrenoreceptor agonists affect the myocardium, creating supplementary tachycardia and contractility but also act to release renin, initiating the RAAS cycle. Beta-2-adrenoreceptor receptors dilate the blood vessels of critical organs as well as the airway to increase oxygenation. Beta-2 pathways also increase glucose production and allow skeletal muscles to contract much more powerfully.
Aldosterone Production
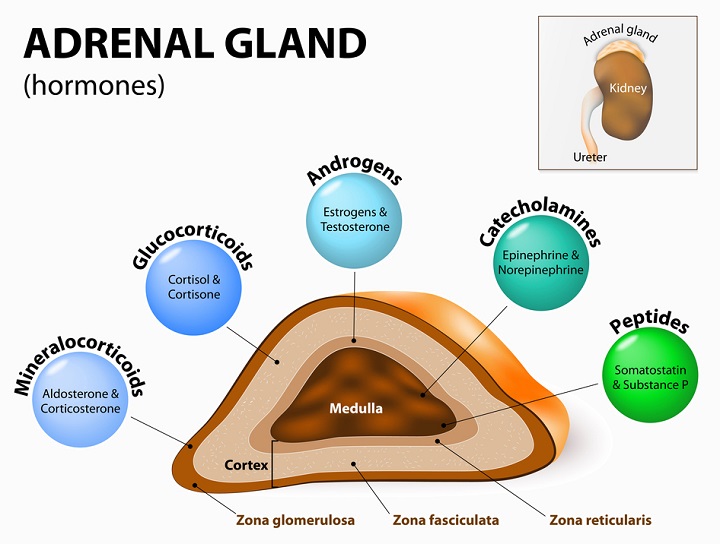
The adrenal glands are situated above the kidneys and are also called the suprarenal glands. They produce a wide variety of endocrine hormones that act as chemical messengers within the confines of the body. Aldosterone is produced in the zona glomerulosa of the adrenal cortex which lies just under the surface. Aldosterone production requires an enzyme called aldosterone synthase. Congenital deficiencies in aldosterone synthase and any other enzymes necessary for aldosterone production lead to hyponatremia and hyperkalemia. This shows that aldosterone primarily maintains correct levels of sodium and potassium within the body
Another ingredient of aldosterone is cholesterol. It is important for hormones to be lipid based so they can easily and rapidly enter the phospholipid membranes of receptor cells. The interaction of cholesterol with a range of enzymes can produce numerous steroid hormones. Steroid hormones or corticosteroids are categorized as mineralocorticoids (aldosterone), glucocorticoids (cortisol), and sex corticoids (estrogen, progesterone, and androgen) according to function. The picture clearly depicts the range of chemicals produced by the adrenal gland and where. In the top right, a small box shows the position of the adrenal gland on top of the kidney.
What is a Mineralocorticoid?
Aldosterone is a mineralocorticoid which means its action is involved in maintaining mineral levels. When activated, aldosterone binds to specific mineralocorticoid response elements (MREs) where they are able to increase the reabsorption of ions and water back into the body and bypass the excretory system. This translates into an increase in extracellular fluids, a higher blood pressure, and lower levels of potassium in the body. As aldosterone is only responsible for small amounts of water, its contribution to extremely high or low blood pressures in the short-term is minimal, but its consistent long-term action on mineral-salt and water balance is crucial. This critical role can be seen in the symptoms of people who suffer from adrenal disease.
Hyperaldosteronism
Overproduction of aldosterone by the adrenal gland is classed as primary or secondary. Primary hyperaldosteronism in both adrenal glands is due to either bilateral adrenal hyperplasia or Conn syndrome (an adrenal tumor) and is rare. Unilateral primary adrenal hyperplasia is even rarer, as is the familial, hereditary form.
Secondary hyperaldosteronism is more common than the primary form but still does not affect a significant percentage of the global population. It is caused by hyperactivity in the RAAS system which is often the result of edema, renin-producing tumors, ascites, and stenosis of the renal artery which leads to low blood perfusion into the kidney even in the presence of normal blood volumes.
The symptoms of primary hyperaldosteronism (or primary aldosteronism) are few but can progress to hypertension, hypokalemia, and hypomagnesemia. Secondary hyperaldosteronism symptoms are similarly spread from asymptomatic to raised blood pressure and lower levels of potassium. More generalized symptoms which are often confused with other illnesses are fatigue, headache, polyuria, polydipsia, and metabolic alkalosis. The aldosterone-to-renin ratio (ARR) blood plasma test is used to differentiate primary from secondary hyperaldosteronism.
Hypokalemia is the result of increased sodium reabsorption in the nephron – an effect which is caused by aldosterone hormone and, in doing so, increases water volume within the body. When sodium is reabsorbed, potassium is excreted. Magnesium levels can be low because the balance of electrolytes within the body is usually co-dependent. Low potassium is often accompanied by low calcium and magnesium levels.
Hypoaldosteronism
Hypoaldosteronism is a similarly rare illness which occurs due to aldosterone deficiency. This deficiency is categorized into hyporeninemic or hyperreninemic hypoaldosteronism – the accompanying levels of renin in the blood. The small numbers of people suffering from this disease are usually kidney patients, diabetics or seriously ill. Other risk factors include lead poisoning and heart medications.
Long-term hyperkalemia, the result of hypoaldosteronism, has a direct effect on the muscles as potassium is necessary for muscle contraction. Low aldosterone symptoms, therefore, include heart palpitations, muscle weakness, and an irregular heartbeat. Others are nausea and difficult-to-control fluctuations in blood pressure.
Blood Pressure Medications
Hypertension medications are categorized into different classes. The general working of the following classes has been discussed at some point in this article, as blood pressure medications work in one or more of the same regions as the RAAS.
ACE Inhibitors
Angiotensin-converting enzyme inhibitors suppress levels of angiotensin, a major component of the RAAS. Lower levels of angiotensin mean less vasoconstriction. ACE inhibitors are teratogenic; meaning the fetus of a pregnant woman taking this medication will also experience low blood pressure, as well as hyperkalemia and kidney failure.
Beta-blockers
By reducing cardiac output, blood pressure is reduced. Beta-blockers lower the rate at which the heart beats and the strength of myocardium contraction. Beta-blockers are known for causing extremely slow heartbeats (bradycardia) of around 30 beats per minute and patients must be carefully monitored.
Angiotensin II Receptor Blockers
Angiotensin II receptor blockers (ARBs) also act upon the RAAS in a very similar way to the ACE inhibitors group. The difference between an ACE inhibitor and an ARB is that the former limits the primary ingredient of angiotensin II production which stops the conversion of angiotensin I to II, while the latter stops the final product from binding to blood vessel receptors. The effect of these two groups is, in essence, the same. However, the longevity of ACE inhibitors and the reluctance of pharmaceutical companies to replace them are creating a lot of debate concerning which of the two is the better choice.
Diuretics
When blood pressures are high due to hypervolemia, usually due to obesity, stress, electrolyte imbalances, low levels of physical activity, chronic alcohol consumption, heart disease, and kidney problems, diuretics can remove excess fluids through sodium excretion. To do this and to avoid specific side-effects, certain groups work at varying levels. This is shown in the picture below, where the actions of the three main groups at different parts of the nephron are shown.
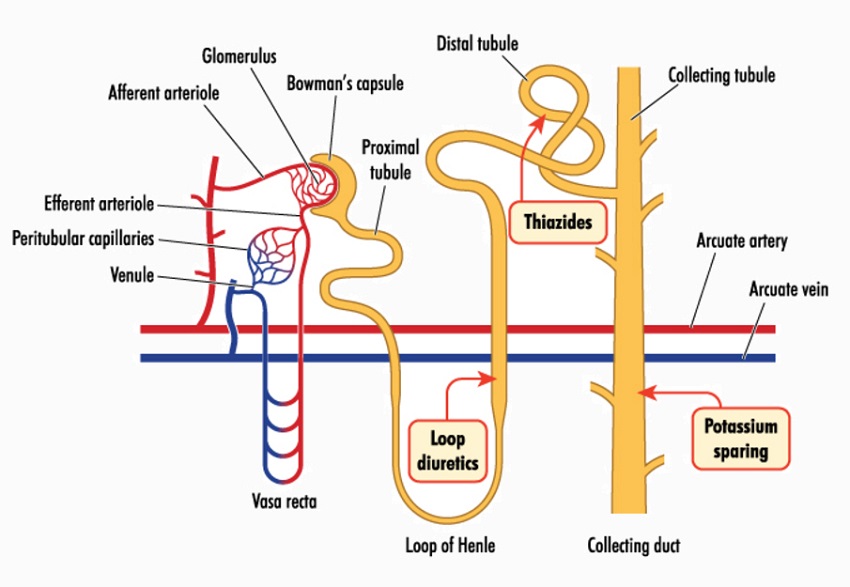
The three main groups are thiazide diuretics, potassium-sparing diuretics, and loop diuretics. Thiazide diuretics inhibit sodium and chloride ion reabsorption early on in the nephron (in the proximal segment of the distal convoluted tubule) but further on, and partially due to the influence of aldosterone on ion cotransporter proteins that allow the passage of salts across the tubular membrane, this effect is somewhat compensated. This compensation is not enough to override the sodium-reducing effect of the proximal segment but does lead to low potassium levels.
Potassium-sparing diuretics, the second group, were developed in answer to the hypokalemia experienced in patients prescribed with thiazide diuretics. These drugs primarily affect the balance between sodium and chloride. More sodium (and more water) is sent to the ultrafiltrate and potassium remains. These drugs, therefore, have the potential to cause hyperkalemia.
The final group is composed of the loop diuretics. These act very early on along the length of the nephron, at the end of the loop of Henlé (hence the name) and before the proximal convoluted tubule. This type of diuretic binds to the cotransporter proteins to slow down or halt sodium and chloride ion reabsorption. This is extremely similar to the mechanism of the thiazides, but the early onset of effects along the tubule means loop diuretics are much more potent. Consequently, thiazides are used to manage high blood pressure in people with a relatively good kidney function; loop diuretics have a better effect in patients with low kidney function and low filtration rates.
Vasodilators
With either a central or local effect, through the vasomotor center of the medulla oblongata or directly on the smooth muscle of the blood vessels, vasodilators increase the size of the blood vessel lumen, creating a larger space in which blood can circulate and lowering the blood pressure. Vasodilators are not a primary therapy for hypertension but used in combination with other blood pressure-lowering drugs. As they also increase blood supply to the heart, vasodilators are primarily used for heart patients.
Combined Alpha- and Beta-blockers
Alpha and beta dual receptor blockers or alpha-beta adrenergic blockers have a double function. As alpha-blockers, they relax the smooth muscle of the blood vessels. As beta-blockers, they slow the heart rate and decrease the strength of myocardium contraction. This double mechanism can create dizziness when standing abruptly or syncope when blood pressure becomes too low.
Quiz