Definition
A P wave on an electrocardiogram represents a phase of electrical activity that causes the atria of the heart to contract. The P wave is a summation wave – electrical activity that comes from successive signaling from multiple points, causing wave-like contractions. These multiple points contain pacemaker cells that generate action potentials independently of the CNS. The P wave is the first wave found on the electrocardiogram of a healthy individual.
What Does the P Wave Represent?
The P wave represents electrical activity (in volts) that causes cardiac muscle contraction in the atria – the upper two heart chambers. When a P wave definition says it represents atrial contraction, this is not entirely incorrect.
What a P wave depicts is the voltage (over time) that specifically triggers atrial muscle cell contraction. An electrocardiogram, therefore, represents electrical activity and not muscle movement.
However, by looking at ECG waves and observing changes or abnormalities in electrical voltage at different points, we can figure out when and which part of the heart muscle is contracting or relaxing and if this is healthy activity or not.
P Wave on the ECG
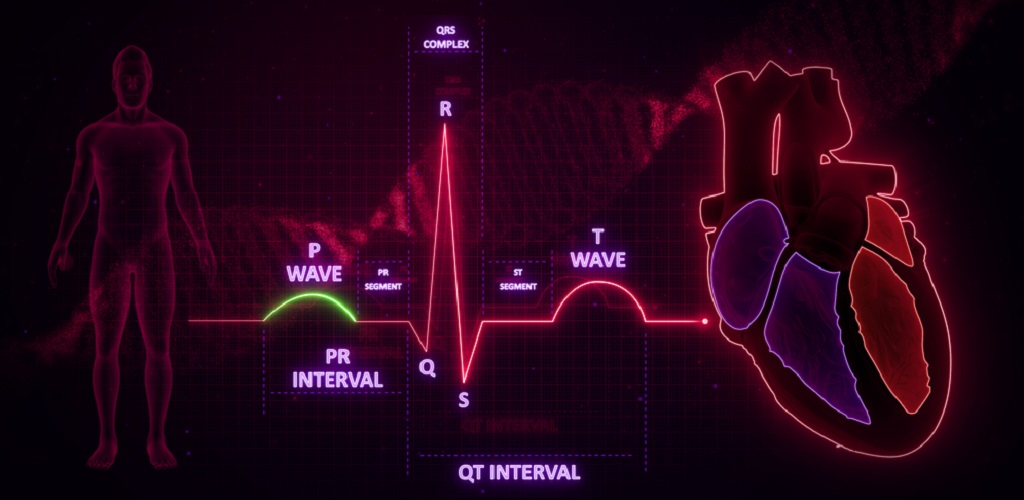
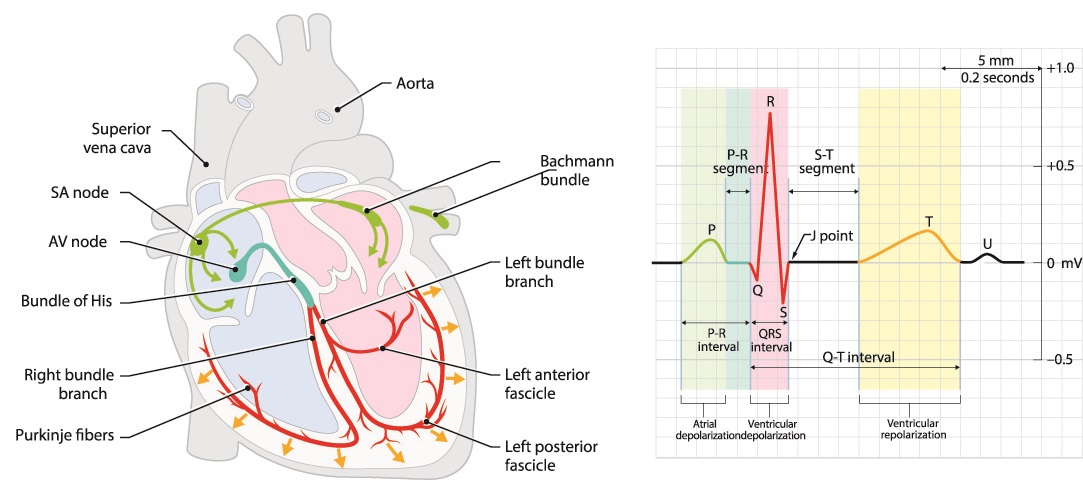
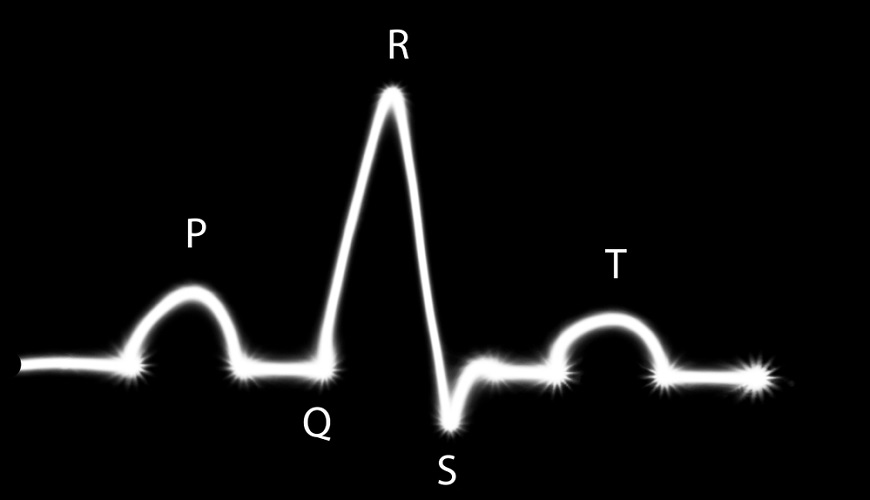
The P wave is the first wave on an electrocardiogram (ECG). It is followed by the PR interval, the QRS complex, the ST interval, and finally the T wave.
By looking at an ECG P wave, cardiologists can translate results into healthy or unhealthy heart function. Abnormal P waves and absent P waves point specifically to problems within the atria.
An ECG, printed on graph paper or on a monitor, depicts voltage and time. A rapid or slow heartbeat is easy to recognize by looking at the intervals between the T wave (the last wave) and the P wave. Irregular intervals or pauses between the P wave and T wave show conductivity problems; these hardly affect the heart rate.

Normal P wave duration is less than 0.12 seconds (120ms) – about 3 squares on an ECG printout. Depending on the number of leads and positioning of the ECG electrodes, the peak of the P wave is between 1.5 mm and 2.5 mm in height. This corresponds with 0.15 to 0.25 millivolts.
P Wave and Conduction
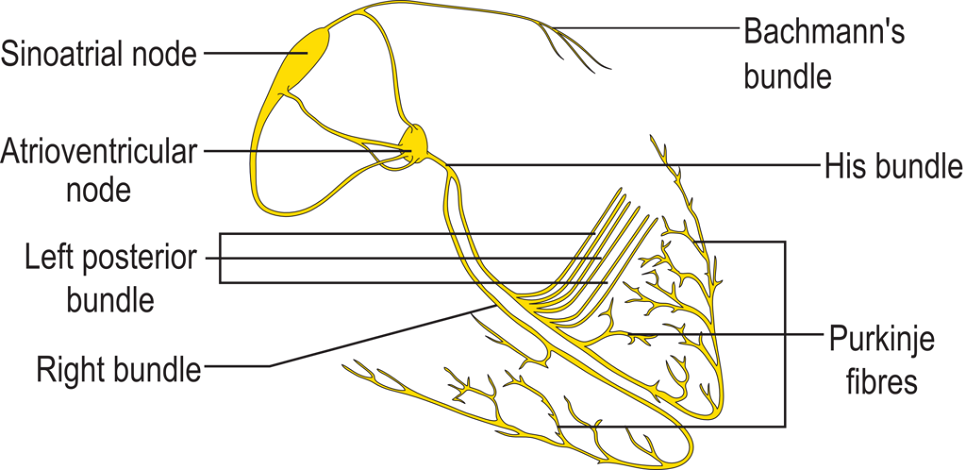
A healthy P wave is initiated in the sinoatrial node of the right atrium. Action potentials generated at this node spread throughout the atria. This means that the right atrium contracts slightly earlier than the left atrium.
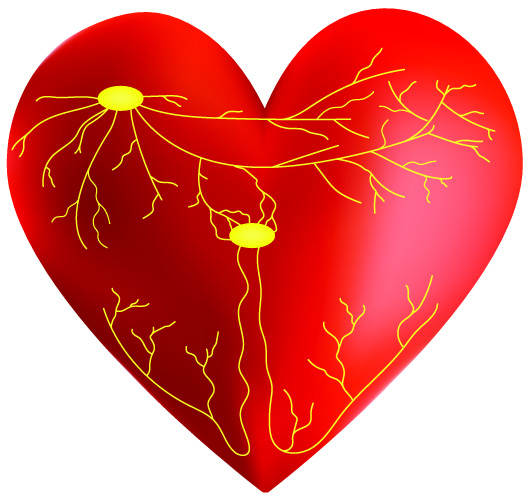
The heart conduction pathway in the atria is composed of the sinoatrial node, Thorel’s bundle, Wenckebach’s bundle, Bachmann’s bundle, and the atrioventricular node. Thorel’s bundle conducts action potentials from the SA node along the back of the right atrium; Wenchebach’s bundle through the right side and front of the right atrium. Bachmann’s bundle is an extension of a group of fibers that cross far into the muscle of the left atrium.
P Wave and Automaticity
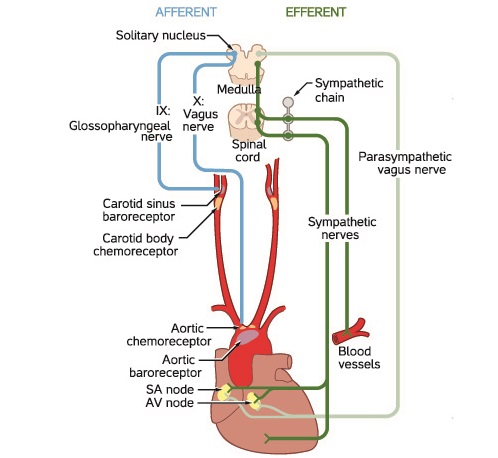
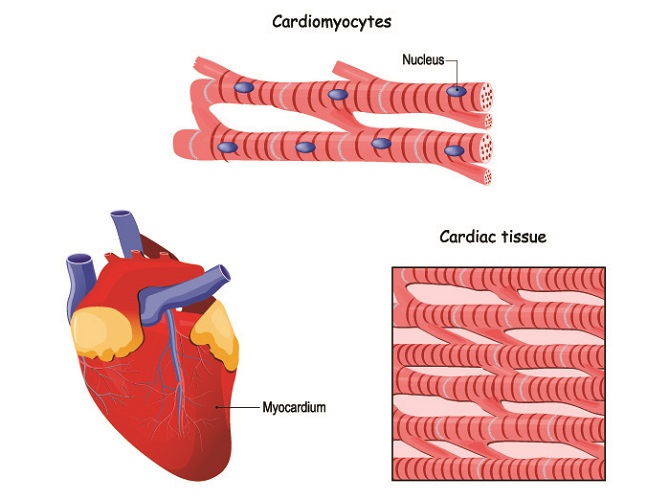
Heart conduction and contraction does not need the brain to function. The medulla oblongata of the brainstem controls how quickly or slowly heart muscle contracts (heart rate in beats per minute) and how much blood is pumped through it; however, the myocardium possesses automaticity. This means that heart cells do not depend on action potentials that arrive from the central nervous system but generate their own.
Specialized pacemaker cells generate action potentials in the heart. These are heart muscle cells (cardiomyocytes/myocardiocytes) with an additional function – action potential generation. Only a very small percentage possesses the ability to produce action potentials.
Pacemaker cells should only be found at the sinoatrial node (SAN) and atrioventricular node (AVN). These cells are the captains of the cardiac pacemaker. Regular (healthy) heart muscle cells do not display automaticity; however, when ions involved in heart muscle contraction (sodium, potassium, and calcium) are imbalanced, regular cardiomyocytes may also start to generate action potentials.
These abnormal signals are ectopic (not coming from the areas where pacemaker cells are usually found). In the atria, P wave abnormalities are often the result of irregular automaticity.
Role of the Central Nervous System
The rate of firing initiated in the SA node is constant – around one hundred times per minute. This is a fixed rate (native rate) and never stops…at least until cardiac arrest. The native heart rate is generated in the heart but adjusted by the autonomic nervous system via the medulla oblongata.
When alarmed, for example, nerves of the sympathetic nervous system override those of the SA node – the heart rate increases. When at rest, parasympathetic nerves override action potential generation in the SA node – the heart rate decreases. The heart rate is regulated by the autonomic nervous system, but the heart will never cease beating (unless large numbers of cardiomyocytes die).
The heart has a backup system: the AV node also contains pacemaker cells. The SA node is the primary pacemaker, but when damaged or malfunctioning the AV node takes over. This is an ectopic rhythm and P waves look abnormal.
Pacemaker cells in the secondary pacemaker – the AV node – also continuously produce action potentials but at a slower rate than the SA node. The faster firings of the SA node overrule the impulses produced in the slower AV node. Because of this, if the SA node malfunctions it is likely that the heart rate will slow down (bradycardia).
Heart Conduction Pathway
Pacemaker cells form and send action potentials from the sino-atrial node at the top of the right atrium. These spread throughout both atria and stimulate the muscle at the top of the heart to contract.
Electrical impulses arrive at the atrioventricular node at the bottom of the right atrium and travel from top to bottom through the bundle of His in the heart septum. The bundle of His splits into a right and left bundle branches; these send action potentials along the right and left side of the septum and through into the right and left ventricle walls respectively.
The right and left bundles eventually become countless Purkinje fibers. Purkinje fibers spread upwards through the muscle of each ventricle. They activate upward contraction to push blood toward the aorta and pulmonary artery.
On an electrocardiogram, the voltages that cause depolarization from the AV node onward form the QRS complex and T wave (see above image).
Electrocardiogram Waves
Electrocardiogram waves show us what is occurring throughout the heart. While this article deals specifically with the P wave, it is still important to get the full picture and understand abnormal P wave pathology.
- P wave: depolarization of the atria. As gravity helps blood to flow into the ventricles, less muscle contraction is required here. This is why the P wave is smaller than the R and T waves.
- PR interval: a short pause before the QRS complex
- Q wave: depolarization of the top of the ventricular septum by the bundle of His. A small, downward-pointing wave.
- R wave: ventricular depolarization at the thickest part of the ventricular walls via the bundle branches – this is why the R wave is the biggest (more voltage is needed).
- S wave: depolarization in the Purkinje fibers. Opposite curve direction to R wave as signals travel from the bottom of the ventricles and move upwards.
- ST-segment: time required for each ventricle to completely depolarize (relax)
- T wave: complete repolarization (relaxation) of the ventricles.
You can test your understanding of electrocardiogram results on the University of Utah School of Medicine website. Tests include heart conductivity anomalies and P wave abnormalities.
P Wave Abnormalities
P wave abnormalities are visible on an electrocardiogram. Most ECG examples in textbooks are relatively clear; in the hospital, a trained eye is usually required.
Inverted P Wave (ECG)
An inverted P wave on an ECG is usually a sign of ectopic atrial rhythm. The action potentials that initiate myocardiocyte depolarization may come from the AV node, from regular cardiomyocytes when certain electrolytes are out of balance, or from ectopic pacemaker cells. An inverted P wave means it is upside down.
Retrograde P wave
If the SA node is not functioning properly, the AV node takes over. The atria still contract because action potentials travel back towards the SA node. The result is a retrograde P wave.
ECG printouts showing retrograde P waves might also cause a cardiologist to suspect a type of ectopic rhythm called junctional rhythm. It often takes longer for the atria to contract, and the P wave might be very close to or within the QRS complex. Retrograde refers to the backward movement of the action potentials.
Notched P Wave
A notched P wave or bifid P wave indicates left atrial enlargement, nearly always the result of a narrowed mitral valve. The mitral valve lets blood flow from the left atrium into the left ventricle. If this valve is narrow – mitral stenosis – the atrium does not have time to empty before it relaxes. When the atria relax, they suck in blood from the venae cavae and pulmonary veins. Mitral stenosis means that the left atrium must stretch (enlarge) to cater for this larger blood volume.
A notched P wave is usually wider (slower) because there is more tissue to pass through. The first half of the P wave before the notch represents right atrial contraction, the second half of the P wave represents left atrial contraction. A sub-type of the notched P wave is the biphasic P wave.

No P Wave on ECG
No P wave on an ECG does not mean the heart has stopped beating – the QRS complex and T wave follow to show the ventricles are still working.
It is possible that the P wave is just extremely irregular and not obvious, such as in atrial fibrillation. Other possibilities are SA node arrest or blockage of the different bundles that connect the SA and AV nodes. If regular myocardiocytes were unable to adapt and generate impulses independently, the result of these pathologies would be death.
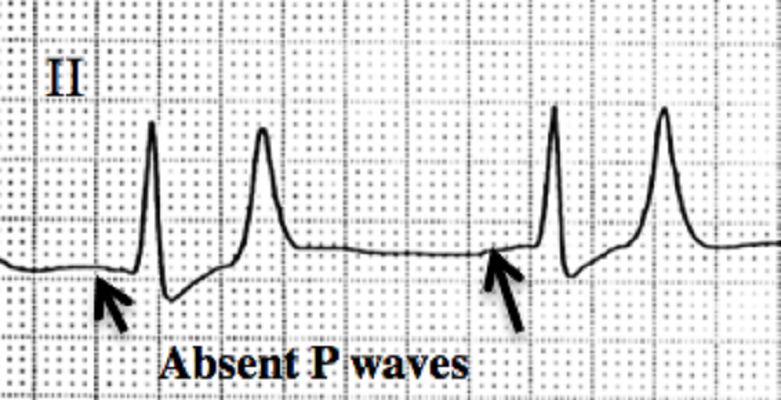
When the SA node stops working, the heart has another trick up its sleeve – escape rhythm. When one part of the heart conductivity system fails, other areas take over. In junctional rhythm, the AV node becomes the primary pacemaker.
If the AV node also fails, an ectopic ventricular beat can be generated by myocardiocytes in the ventricles. These need a second or two to generate, so the heart rate becomes very slow – twenty to forty beats per minute. Without atrial electrical activity, there is no P wave on the ECG or monitor.
Atrial Flutter
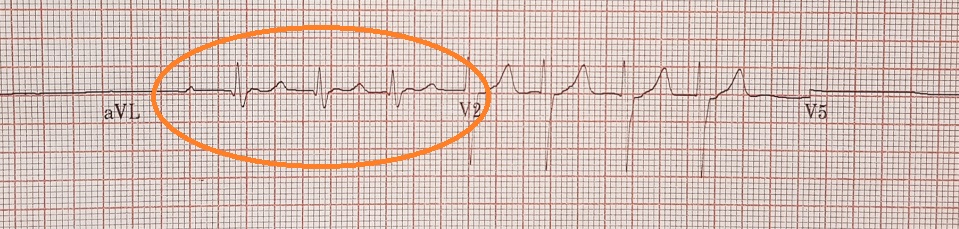
Atrial flutter may sound like a fatal disorder but is quite common. Multiple P waves and a rapid heart rate are characteristic. This pathology can progress to become atrial fibrillation.
In atrial flutter, the atria contract more than once. As most blood moves from the atria to the ventricles via gravity, these multiple contractions are not as dangerous as you might think. Even so, atrial flutter causes turbulence and small blood clots can develop.
Flutter P waves on ECG printouts are close together – rates of up to three hundred beats per minute are possible. The ventricles do not contract at the same rate – usually at less than half of the rate of the atria. Atrial flutter rhythm, apart from being too fast, is regular. The P waves (plural) have a typical saw-tooth pattern.
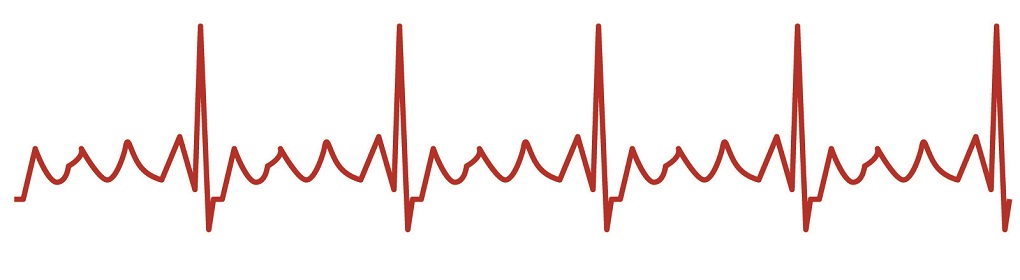
Atrial Fibrillation
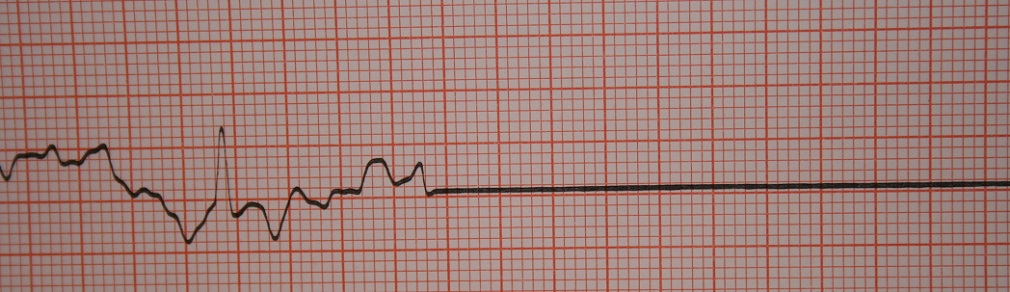
Atrial fibrillation or AFib affects up to 6.1 million people in the US. It can cause symptoms or be silent (without symptoms).
The differences between atrial flutter and atrial fibrillation are the rhythm and appearance of the P wave. In AFib, rhythm is irregular and P waves are shallow, wobbly lines – the untrained eye might think there is no P wave on the ECG.
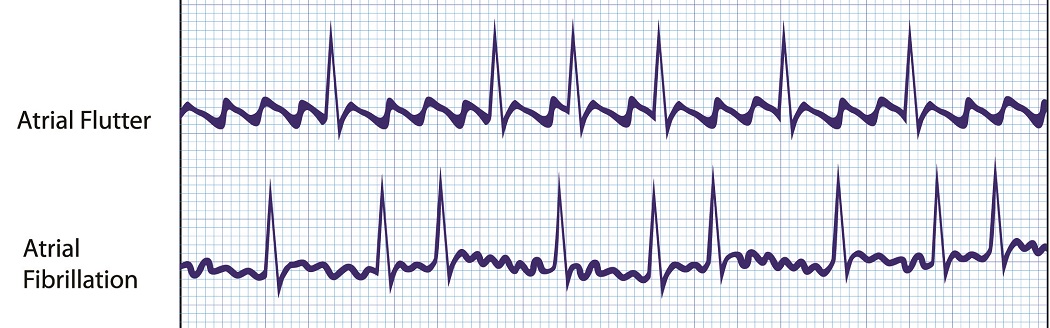
Atrial fibrillation is caused by multiple ectopic action potentials coming from various areas dotted around the atria. Approximately one-third of people with AFib also suffer from atrial fibrillation.
AFib has a higher risk of blood clot formation. The heart rate is also rapid but the pulse is more often than not irregular; this is not always the case in mixed flutter/fibrillation pathology.
Quiz