Definition
The kidney is a paired vital organ that removes waste products from the blood and regulates fluid and electrolyte levels within the body. Only one is necessary, but this organ’s importance means that we have two; should one shut down, there is a backup. Kidneys contain numerous nephrons – miniature filtration systems that regulate salt, water, glucose, and amino acid levels in the blood plasma filtrate that eventually becomes urine. The kidney also secretes two hormones, renin and erythropoietin.
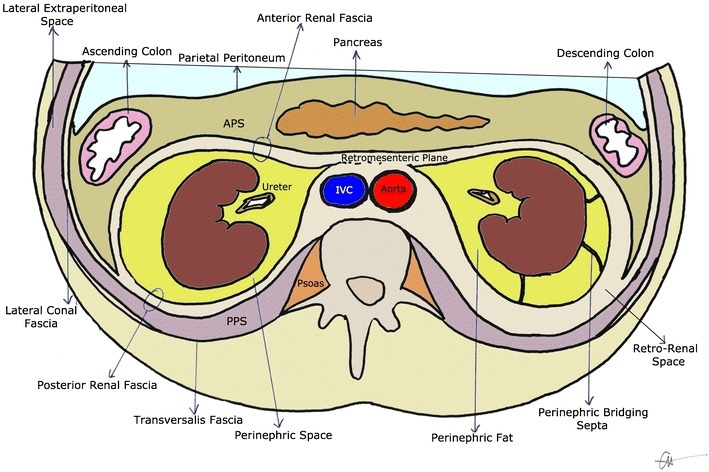
Kidney Location
The kidneys are located at waist level and at the posterior (back) wall of the abdomen. They are partially covered by the ribs. In around 95% of cases the left kidney is positioned at a slightly higher position than the right. When the right is higher than the left, other pathologies may be present.
Each kidney is protected by the rib cage, perirenal (perinephric) fat, renal capsule, and the muscles of the back. These vital organs do not lie within the abdominal cavity but sit behind the peritoneum – they are retroperitoneal.
Kidney Anatomy
Kidney anatomy nearly always describes these organs as bean-shaped – this is where the name for the kidney bean comes from; both shape and color are similar.

Human kidneys are approximately ten centimeters in length and five in width. Together with the ureters, urethra, and bladder they form the urinary system.
Each organ is covered in a tough membrane called the renal capsule. This membrane keeps the soft inner tissue in place and provides an extra layer of protection. Outside this capsule is a layer of fat – the perirenal fat capsule. This fat layer is covered by the renal fascia.
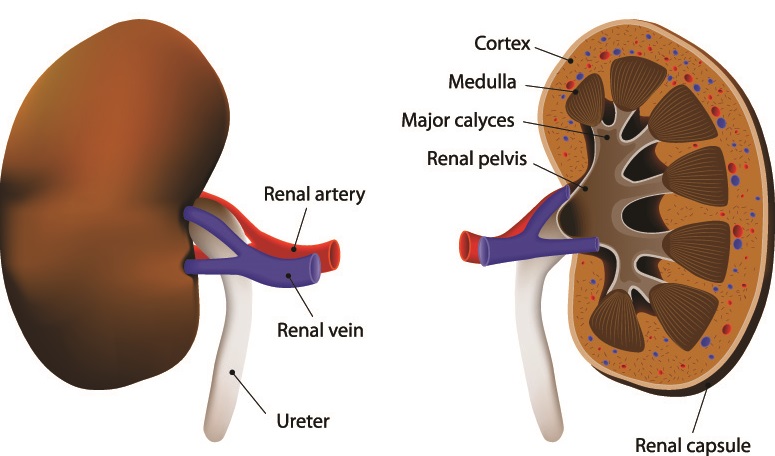
Kidney anatomy begins at the renal hilus, also called the renal hilum or pedicle. This is the indentation that produces the bean-like form. It is where the renal arteries, renal veins, and the hollow, muscled tube of the ureter access the inner tissue.
If you cut vertically through the kidney of any animal you will find the same basic structures as can be seen in a human specimen. Close to the hilus is a white area of tissue. This is surrounded by almost triangular blobs. The outer edge of a freshly-dissected kidney is a deep, reddish-brown.
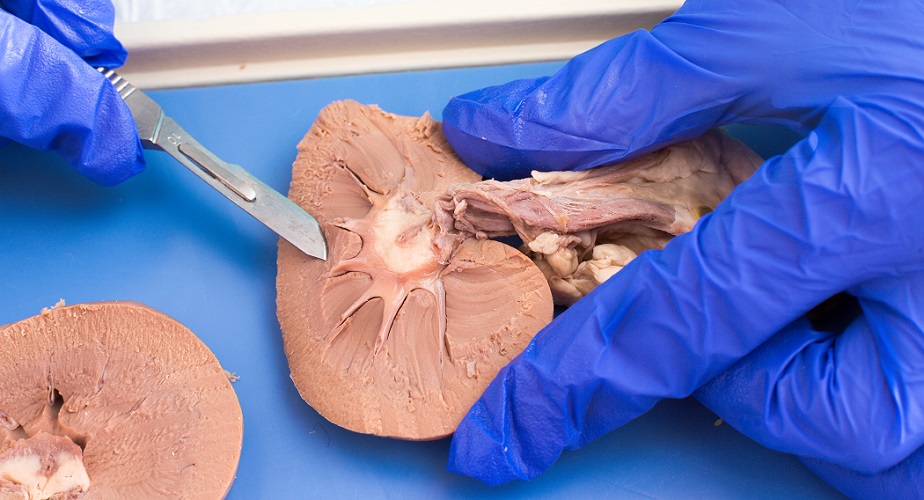
Pelvis
The white tissue as can be seen in the above image is called the renal pelvis, pelvis renalis, or pyelum. The word pelvis means basin – in this case, a fluid collection and drainage point. The pelvis is a funnel system that brings newly-created urine to the ureter from the calyces.
Medulla
The renal medulla is the next functional area and is recognizable by the shape of the renal pyramids. Nephron loops, portions of the convoluted tubules, and collecting ducts are housed within the pyramids. Pyramids drain urine into the calyces and these bring urine into the renal pelvis; all urine leaves the kidney via the ureter.
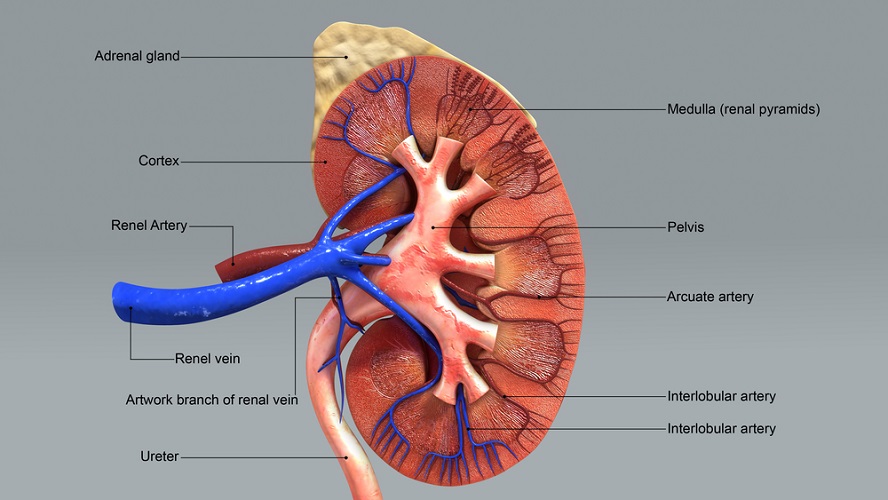
Cortex
The third functional structure is the renal cortex that contains the Bowman’s capsules, glomerulus (capillary network), and portions of the convoluted tubules of nephrons. Interstitial cells in the renal cortex also produce the hormone erythropoietin (EPO).
Renin-producing cells are found both in the medulla and cortex, close to the nephrons. These secrete a hormone called renin that plays an important role in blood pressure regulation.
Blood Supply
Blood arrives at the left and right kidneys via the left and right renal arteries respectively; these are branches of the abdominal aorta (the thick, central artery in the image below). The aorta brings oxygenated and nutrient-rich blood to the organ; however, this blood also contains waste products.

At the hilus, the renal artery splits into arterioles and then countless capillaries. Capillaries are thickly spread throughout the kidneys and also form tightly-wound networks (glomeruli) at the start of each nephron.
Nephrons
Nephrons are individual filtering systems; the average human kidney contains between 200,000 and more than 2.5 million nephrons. No new nephrons are formed from around the 36th week of gestation.
Waste products remain in the blood plasma filtrate as it makes its way through the length of a nephron. The final solution – urine – passes into collecting duct networks that merge into single openings (renal papillae) at each pyramid base. From these papillae, urine passes into the calyces.
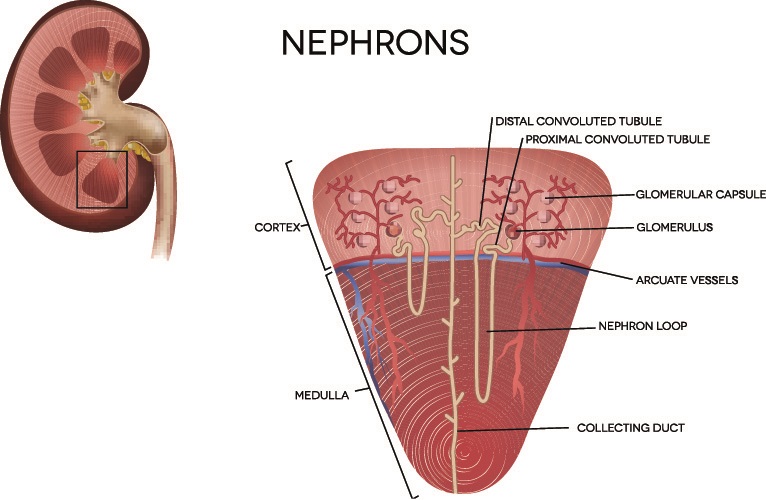
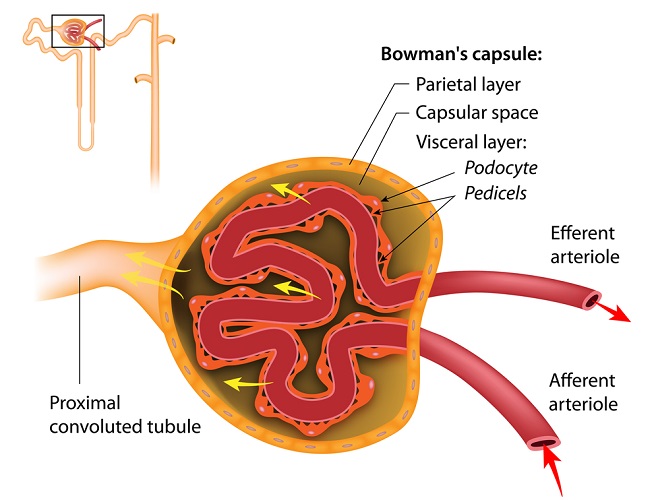
Nephrons are divided into two units – the renal corpuscle and renal tubule. The corpuscle describes the capillary group (glomerulus) and Bowman’s capsule. These are positioned inside the renal cortex. The Bowman’s capsule absorbs filtrate from the glomerulus via passive transport. This is the filtration phase of urine production.
Nephron tubules absorb and secrete different small molecules and ions at specific locations. The action in which molecules enter the tubules via the Bowman’s capsule and interstitial tissue is called absorption. Molecules that return to the interstitial fluid from the filtrate is called reabsorption. Secretion is the addition of other products into the tubular fluid that help the kidneys regulate pH and electrolyte levels. Excretion is the transfer of water, ions, creatinine, toxins, and urea – the components of urine – into the collecting ducts.
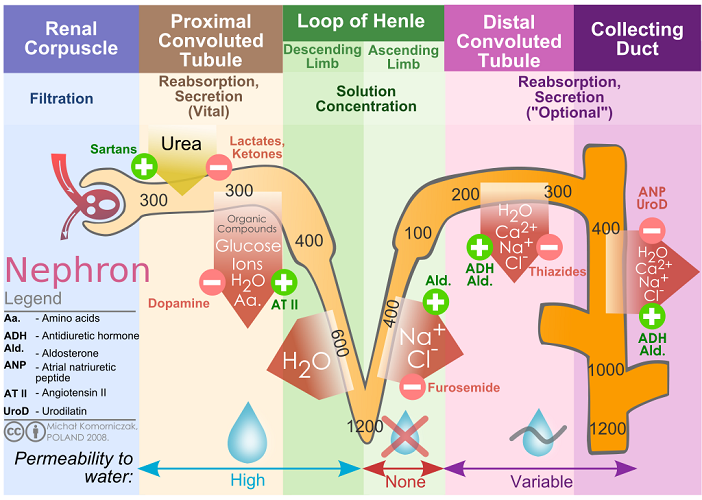
The Bowman’s capsule is attached to the proximal convoluted tubule. This area allows sodium and chlorine ions, water, amino acids, glucose, and vitamins to be reabsorbed into the blood. Hydrogen and potassium ions, phosphate, citric acid, ammonia (NH3), and urea are absorbed into the tubule from the interstitial tissue.
The descending and ascending loop of Henlé is located in the kidney medulla. The descending loop primarily allows water reabsorption. The ascending loop absorbs chlorine and sodium ions, as well as urea from close-lying collecting ducts. The ascending loop of Henlé is impermeable to water molecules.
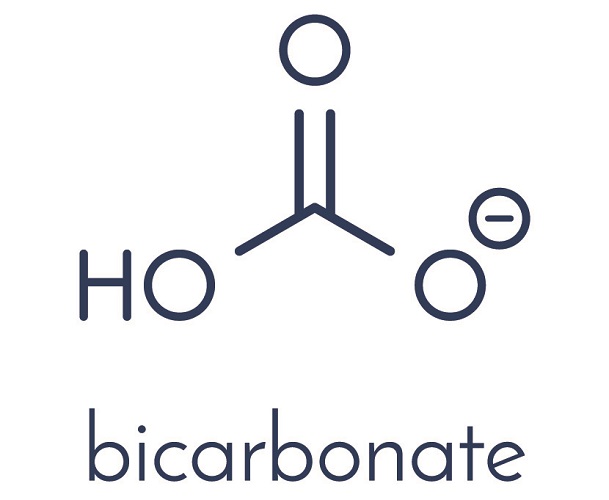
The distal convoluted tubule exits into a collecting duct and allows salt (NaCl), calcium ions, and water to be reabsorbed. The tubule absorbs bicarbonate, hydrogen and potassium ions, and ammonia. Hydrogen and bicarbonate must be well-balanced to ensure the body’s pH. The pH of arterial blood is between 7.35 to 7.45 – an extremely narrow range.

Absorption and reabsorption require both passive and active transport mechanisms.
Kidney Function
Kidney function is not just the removal of waste products, although this is incredibly important. Without at least one functioning kidney we would die without medical intervention.
Fluid Balance
As already mentioned, the loop of Henlé is important for fluid regulation (water homeostasis). All of our blood is filtered – on average – fifteen times a day. When we are dehydrated the descending loop of Henlé absorbs less water and lets water molecules be reabsorbed into the interstitial tissue. Any urine will be darker in appearance.

Water homeostasis in the kidney is regulated by antidiuretic hormone (ADH) secreted by the pituitary gland. When water levels are low, ADH increases water reabsorption in the descending loop of Henlé.
Blood Pressure Regulation
Kidneys are part of the renin-angiotensin-aldosterone system (RAAS) that controls blood pressure and fluid balance. The regulation of blood pressure has much to do with fluid levels; however, unlike fluid balance that is predominantly under the influence of ADH, blood pressure regulation depends on other hormones.
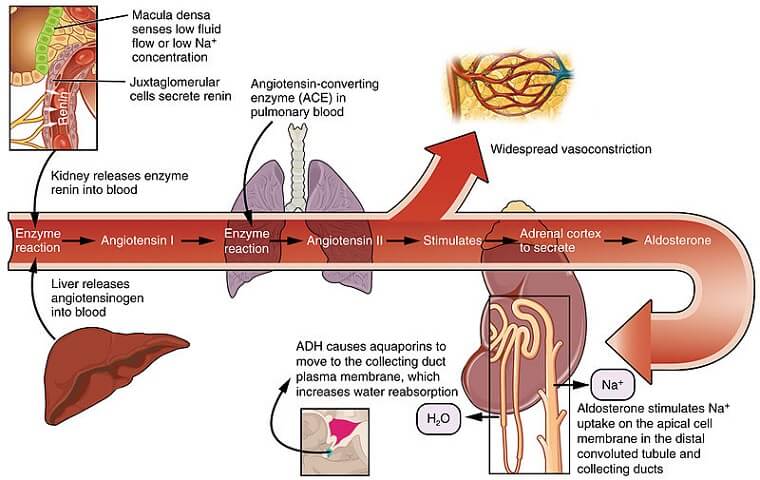
Renin is the first step in the RAAS system. Low levels of sodium or a low blood volume triggers renin release from the kidney cortex. Renin is required to convert angiotensinogen in the liver to angiotensin I. A further enzyme – angiotensin-converting-enzyme – is produced in the lungs and converts angiotensin I into angiotensin II. Angiotensin II causes vasoconstriction in the peripheral blood vessels to increase blood pressure.
At the same time, angiotensin II triggers the secretion of aldosterone from the adrenal glands. Although the adrenal glands are positioned above the kidneys, they are separate organs. Aldosterone tells the nephrons to let sodium and water be reabsorbed into the interstitial tissue and to excrete potassium into the urine.
Electrolyte Balance
Athletes are often seen consuming drinks with added electrolytes. Sweating excretes essential minerals dissolved in water (electrolytes). This loss also occurs during bouts of vomiting or diarrhea.

The most common electrolytes in the body are sodium, chloride, potassium, magnesium, phosphate, and bicarbonate. Each of these minerals has multiple essential roles.
Sodium and chloride have a strong affinity for water and healthy kidneys are very good at removing excess salt from the body. If you eat a very salty meal you are likely to feel thirsty and need to go to the toilet within a short time. This is because the kidneys excrete the components of salt and salt brings a lot of water with it. The extra water fills the bladder and the lack of reabsorbed water stimulates the release of antidiuretic hormone that makes you feel thirsty.

Sodium and chloride are also essential for cell signaling and muscle contraction. Sodium and potassium have opposite effects and when unbalanced are associated with cardiovascular disease. Phosphate is an important mineral for the bones, teeth, nerves, and muscles. Magnesium is associated with over 300 different biochemical reactions in the body.
Bicarbonate is a natural alkali that helps to adjust the pH of the body. Carbon dioxide and hydrogen ions are acidic; while we can breathe out carbon dioxide, other acids need to be neutralized or removed. Alkaline bicarbonate ions and acidic hydrogen ions form the basis of pH homeostasis in the body; these can be absorbed in or reabsorbed from urine.
Toxin Removal
Together with the liver, the kidneys do their best to protect us from toxins. Bites from venomous snakes cause the blood to clot; components of the clotting mechanism gather in kidney collecting ducts. Even when promptly treated, poisoning can lead to acute kidney injury or permanent kidney failure.

Toxins can be small, medium, or large molecules. Large molecules and most cells are too big to pass into a healthy Bowman’s capsule; instead they stay in the blood. The liver breaks these molecules down into smaller ones.
Toxins can be any waste product – broken down dead cells and cell respiration byproducts, for example. A huge range of toxins leave the body via the urine.
Damaged nephrons are highly permeable – the appearance of larger protein molecules in the urine such as albumin and/or red blood cells often tells us that one or both kidneys are damaged.
Erythropoietin Production
Erythropoietin or EPO is a hormone that increases red blood cell production.

When the body detects lower oxygen levels in the body, more red blood cells are produced to transport available oxygen to the tissues. At sea level, the air contains around 21% oxygen; at 6,000 feet this is reduced to just 9.5%. People living in high altitudes have more red blood cells.
Some professional athletes illegally use EPO to increase oxygen supply to the muscles. In 2009, the Moroccan runner Mariem Alaoui Selsouli was banned from the sport for two years for taking EPO. The Italian marathon runner, Roberto Barbi, has been banned for life after having been tested positive for EPO in 2001 and 2008.

Vitamin D Activation
The kidney plays an essential role in the vitamin D activation pathway. Obtained from the diet or after exposure to the sun, vitamin D is transported to the liver where it is converted into calcidiol. Healthy kidneys have many receptors for calcidiol and convert it to an active, useable form of vitamin D called calcitriol.
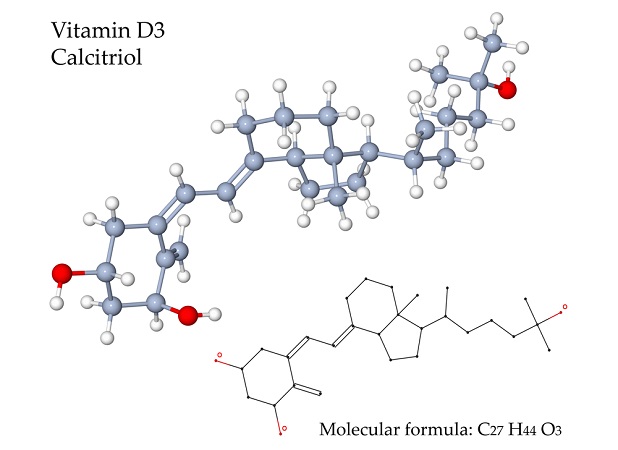
Calcitriol is essential for bone health, calcium absorption, cell growth, muscle function, and immunity. People with chronic kidney disease sometimes require calcitriol supplementation – there is no point in giving them the inactive form of vitamin D as it is the kidneys that turn the inactive form into the active form.
Kidney Disease
Kidney diseases and disorders are common – the many tiny components can easily become damaged and as a vital organ, any problem with the blood supply can end in disaster.
Kidney Infection
Kidney infections are usually the result of untreated or resistant lower urinary tract infections. Infection reduces kidney function and causes extreme pain. Kidney infection treatment is usually specific (narrow-spectrum) antibiotics.

Kidney Stones
Kidney stones or renal calculi are mineral deposits, often produced when certain foods are consumed with too little water or in combination with diuretics. Small kidney stone symptoms are few; they are excreted during urination. Passing a kidney stone in this instance is painless.
If it is not flushed out, further mineral layers can increase the size of a kidney stone. Symptoms develop into excruciating back, flank, and lower abdominal pain on one side (the affected side) of the body. This pain is the result of blockage and high pressure inside the organ; kidney infection due to stagnant urine is possible. A kidney stone that blocks urine excretion is a medical emergency.

Exactly what causes kidney stones, or at least the most common culprits, are calcium, oxalate, and uric acid. In large quantities and without sufficient water to dissolve them, crystals link together to form kidney stones. Treatment for larger crystals is via soundwaves (lithotripsy) that break them without the need for more complex and invasive actions. If this is unsuccessful, surgical extraction is required. After surgery a kidney stent may be inserted to keep the affected ureter dilated; future stones will be less likely to cause a blockage.
Foods that cause kidney stones include oxalate and phosphate-rich items like cola, nuts, beans, beer, chocolate, organ meat, poultry, and dark leafy vegetables.
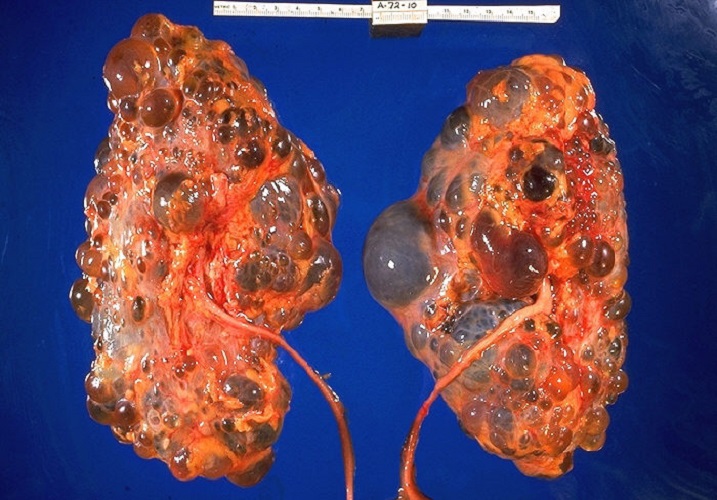
Polycystic Kidney Disease
Another disorder associated with these vital organs is polycystic kidney disease (PKD). PKD is an autosomal dominant genetic disorder that affects up to one in every thousand people. Polycystic kidney disease describes fluid-filled cysts that form on and in the kidneys. Symptoms include chronic high blood pressure and excessive waste products in the blood. PKD can lead to kidney infection, injury, failure, or cancer. The only ‘cure’ is a new kidney; many patients join kidney transplant waiting lists.
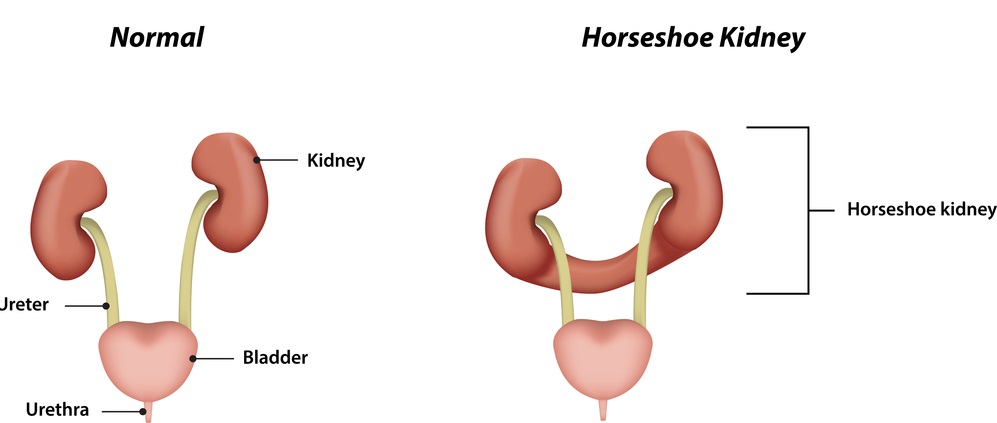
Horseshoe Kidney
A horseshoe kidney is the result of joined kidneys that produce a horseshoe shape. It is relatively common – around one in 500 children are born with this congenital disorder. Horseshoe kidney symptoms include abdominal pain, nausea, and a higher risk of kidney stones and kidney infections. It is also thought that someone with a horseshoe kidney has a higher risk of developing kidney cancer.
Kidney Cancer
Kidney cancer is relatively common. The American Cancer Society reports that there is a higher risk between the ages of 65 and 74. Men are more likely to develop kidney cancer, especially if they smoke, are obese, or suffer from chronic hypertension.
Acute Kidney Injury
Acute kidney injuries develop quickly, perhaps through trauma, untreated infection, and last for a few hours to a few days. Even so, it is often necessary to take over the filtration function of the kidney for this period by way of hemodialysis.

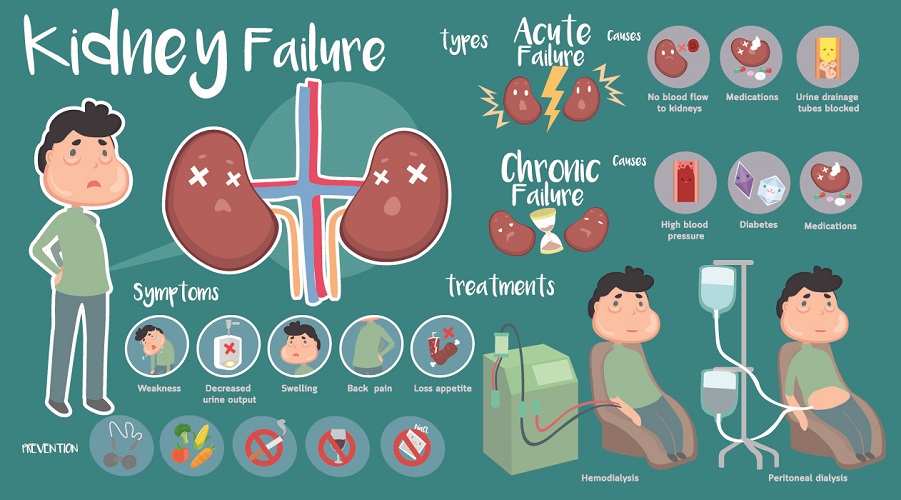
Kidney Failure
Kidney failure in both kidneys can be caused by acute or chronic kidney disease. If only one kidney fails, the remaining kidney – when healthy – can carry out all functions on its own. If both kidneys are damaged, the person will require hemodialysis or peritoneal dialysis. Waiting times for a healthy, tissue-matched kidney are about five years. During this time, regular dialysis (three times a week) is necessary.
Quiz

