Definition
The fallopian tube(s) – also known as “uterine tubes” or “oviducts”- are two hollow ducts in the female reproduction system where oocyte fertilization occurs. There are two tubes present in the system, where each extends from the uterus in the right and left directions and ends near the right and left corresponding ovaries. The fallopian tubes do not directly connect to the ovaries, and instead connect to fimbriae that catch released oocytes during ovulation. Following oocyte fertilization by sperm, the now zygote exits the fallopian tubes and implants itself along the uterus lining. The fallopian tubes are a common site for disorders- such as ectopic pregnancies- and infections- such as with sexually transmitted diseases. They also offer a convenient location to perform voluntary sterilization in women who do not wish to have children.
Background of the Fallopian Tubes
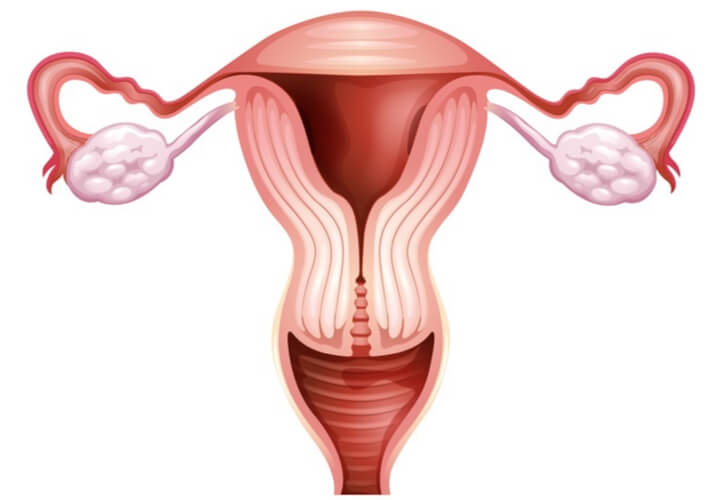
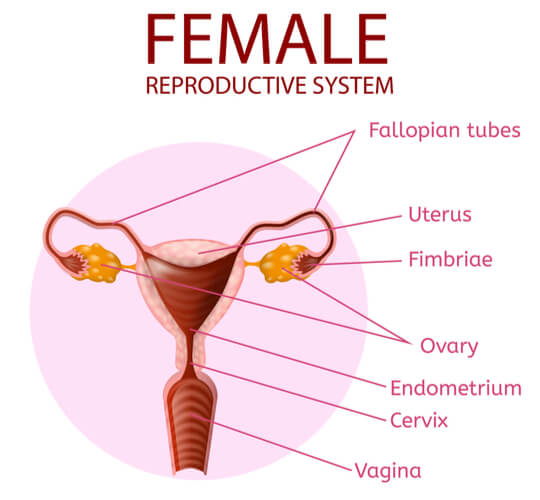
Location and Structure
Females have two fallopian tubes in their reproduction system that are ~10cm long and extend from the uterus towards the right and left ovaries. Specifically, they extend off of the uterine horns of the uterus. However, the fallopian tubes do not make direct contact with the ovaries. Instead, they end near the ipsilateral ovaries, where a specific fimbria- known as the fimbria ovarica– forms a connection from the end of the fallopian tube to the ovary. The cells of the fimbriae contain cilia (which are small hair-like projections that stem off the cells), which create a current towards the fallopian tubes.
The fallopian tubes themselves consist of four sections, including the uterine, isthmus, ampulla, and infundibulum regions. The uterine region is closest to the uterine horns, with the isthmus region being the next section away from the uterus. The ampulla is the third region from the uterus and is commonly the location of oocyte fertilization. The infundibulum is the final region, which ends at the abdominal ostium and leads into the fimbriae and peritoneal cavity.
Function
The fallopian tube’s primary function is to accept oocytes (the immure egg, which are the female gametes) from the ovaries. As mentioned previously, there is not a direct connection between the fallopian tubes and the ovaries. Instead, the fimbriae at the end of the tubes catches the oocyte and the cilia on the fimbriae guides it into the fallopian tubes. Because there is no direct connection between these two major structures, either ovary can release the oocytes into either fallopian tube. Generally, the oocytes are projected from the ovary into the overall peritoneal cavity. Due to this projectile, only a portion of oocytes actually reach the cavity. Peristalsis (which is the wavelike movement in smooth muscle) of the fallopian tubes carries the oocyte in the direction of the uterus.
The oocytes do not immediately move into the uterus. Instead, the oocytes remain in the fallopian tubes, where they become fertilized if sperm (the male gametes) is present. If fertilization does occur, peristalsis of the fallopian tubes then moves the fertilized oocyte (now called a zygote) into the uterus, where the zygote is able to implant itself to the uterine lining. By hosting the fertilization process, the fallopian tubes also provide nourishment through the non-ciliated cells present in the tubes.
The Fallopian Tube’s Role in the Ovarian Cycle
It has been assumed that females have all of their oocytes upon birth. (However, some research may challenge this assumption, as data shows that it may be possible for epithelial cells to create stem cells at the ovary’s surface.) At this point, the oocytes are known as primary oocytes, and they remain at prophase 1 of meiosis until the female reaches puberty. Once puberty occurs, the ovarian cycle begins.
There are three phases of the ovarian cycle: the follicular phase, ovulation, and the luteal phase. The overall cycle takes around ~28 days on average. While the follicular phase varies in length between females, the luteal phase typically lasts 14 days.
The Follicular Phase
Following puberty, a few selected primary oocytes become activated each month, where one will eventually become the dominant primary oocyte. This is the oocyte that will continue through the subsequent steps of meiosis 1 in order to create two daughter cells. Of the two daughter cells from the dominant primary oocyte, one will become the secondary oocyte and the second will become the first polar body. (The first polar body may or may not continue into meiosis II to form two more polar bodies, but all polar bodies will eventually deteriorate regardless). These steps constitute the follicular phase and occur in the ovaries. This phase is named as such because it also constitutes the growth and maturation of the follicle cells surrounding the oocyte.
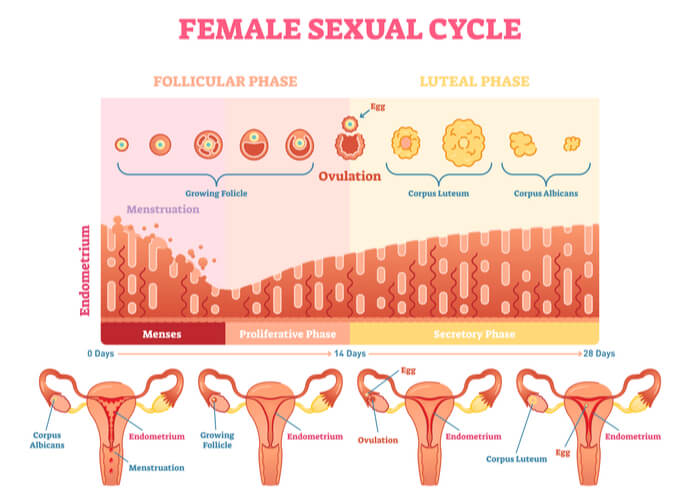
Ovulation, the Luteal Phase, and Menstruation
The secondary oocyte surrounded by mature follicle cells is released from the ovaries and enters the fallopian tubes during ovulation. The secondary oocyte then waits at metaphase II of meiosis while the mature follicle cells rupture to form a structure known as the corpus luteum. The corpus luteum is responsible for releasing progesterone and estrogen hormones to support an expected pregnancy for the first three months (until placenta formation). If no sperm is present at this stage, then these structures will break down while still in the fallopian tube. These steps constitute the luteal phase (named as such due to the follicular formation of the corpus luteum).
Following the 14-day period in which the corpus luteum degenerates, the menstrual cycle (in human and non-human primates) or the estrous cycle (in most other mammals) occurs. Both of these cycles include the shedding of the uterine walls which thickened over the course of the ovarian cycle in preparation for an expected pregnancy. However, the menstrual cycle is differentiated by external bleeding from the uterus and into the vagina as a result of the shedding. The estrous cycle does not include external bleeding, as the uterine lining is instead reabsorbed. The menstrual and estrous cycles mark the beginning of the ovarian cycle, before follicular phase occurs once again and the cycle repeats.
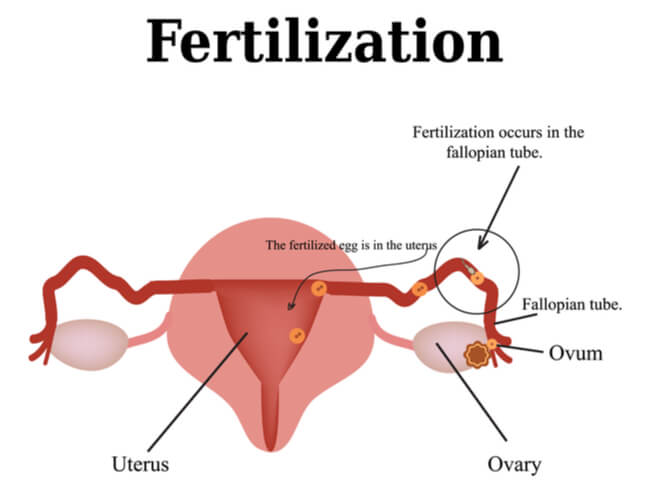
Fertilization
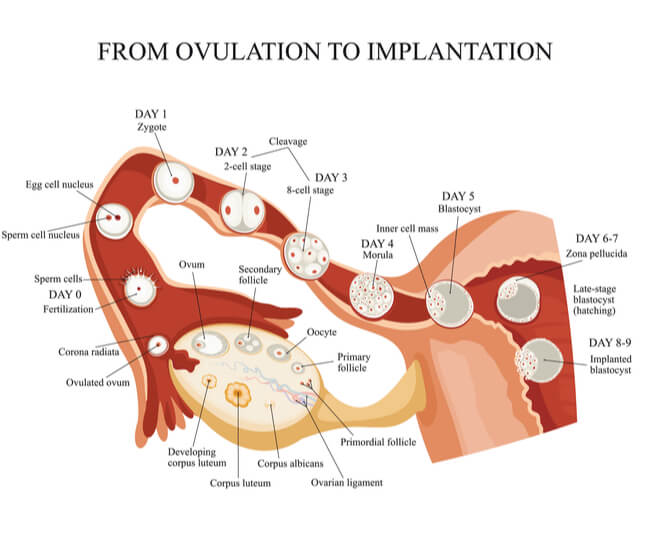
On the contrary, if sperm is present and fertilizes the secondary oocyte while in the fallopian tubes, the now fertilized oocyte (called a zygote) will complete the remaining steps of meiosis II. Another polar body will be created along with the fertilized oocyte following meiosis II. However, this polar body should also deteriorate as the previous ones did. In normal pregnancies, the zygote will relocate from the fallopian tubes and into the uterus, where it will implant itself along the uterine wall and continue through the developmental process.
Diseases and Disorders of the Fallopian Tubes
The fallopian tubes can be affected by diseases, which can lead to symptoms that cause disorders that range in severity. As part of the female reproductive tract, these diseases tend to be sexually transmitted. Additionally, given their importance in oocyte movement and fertilization, the fallopian tubes are a common location where infertility-related issues can arise. Alternatively, they offer a convenient location for voluntary sterilization. Voluntary sterilization can be safely done by tubal litigation, which has been shown to be highly effective and permanent.
Salpingitis
Salpingitis is the inflammation of the fallopian tubes. Inflammation is nearly always caused by microbes, with these microbes usually being from strains that cause sexually transmitted diseases (or STDs). The former most common microbe was Neisseria gonorrhoeae, which is commonly known for causing gonorrhea. Gonorrhea has been declining over recent years, and now non-gonococcal organisms- such as Chlamydia trachomatis, which causes chlamydia- are the common causes of inflammation. Salpingitis can also present itself alongside additional symptoms, such as fever, lower abdominal and pelvic pain, and pelvic masses.
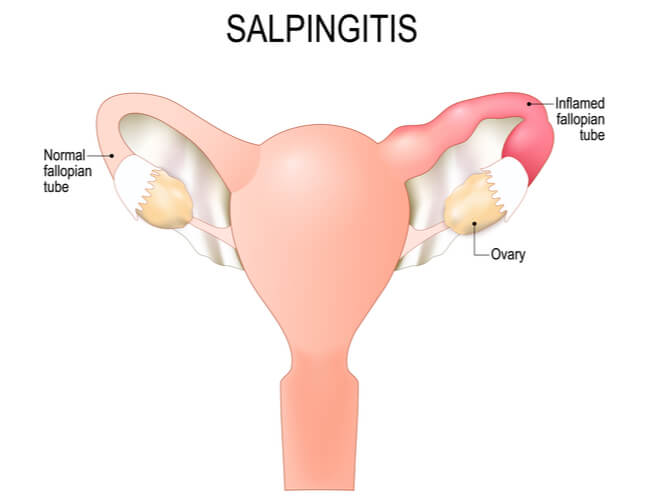
During salpingitis, the now inflamed tube can adhere to the ovaries and adjacent tissues, causing a tubovarian abscess to occur. Additionally, the tubes can adhere to the tubal plicae, which can increase the chances of ectopic pregnancy (where fertilized zygotes are implanted in parts outside of the uterus) in the fallopian tubes. The fallopian tubes are the most common location for ectopic pregnancies, which occur in about 1% of pregnancies. These pregnancies typically abort themselves spontaneously, but the ones that do not abort are usually not detectable until a rupture occurs. Once the rupture occurs, severe symptoms can result- including abdominal pain, acute abdomen, and shock- where surgery is required immediately to avoid exsanguination and/or death. Damage to the lamina of the fallopian tubes can additionally result in permanent sterility.
STDs: Gonococcal Infections
Gonococci organisms- such as N. gonorrhoeae- cause STDs that present similar morphology in both males and females. The most common symptom includes urethral exudates (or fluid leakages from the tissues), but these tend to be heavier in males and less noticeable in females.
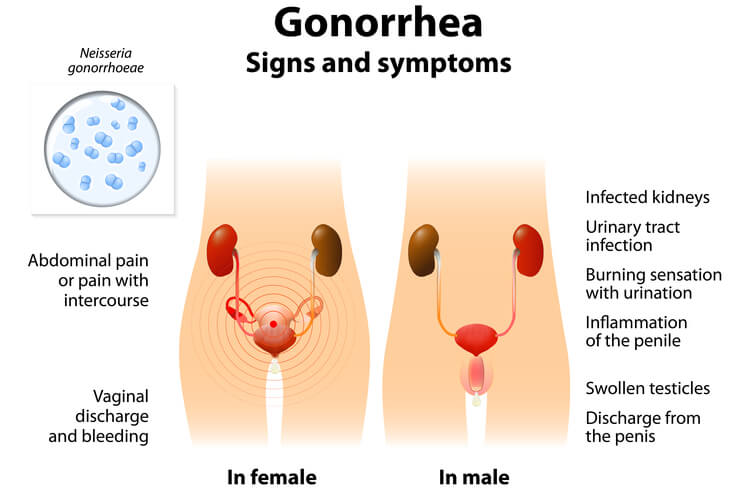
Initially, females with gonorrhea can either show no symptoms, or show signs of dysuria, lower pelvic pain, and vaginal discharge. If left untreated, the infection can ascend into the uterus, fallopian tubes, and ovaries. This can lead to acute salpingitis, which can then turn into tubovarian abscesses. Eventually, this can result in scarring that can lead to permanent deformities of these structures. These deformities can further result in ectopic pregnancies, infertility, and pelvic inflammatory disease. Additionally, pregnant women infected with gonorrhea can pass the disease to their newborns, which can result in blindness of the infant.
Traditionally, gonorrhea has been treated with antibiotics. However, such as with many infectious microbes, N. gonorrhoeae has been becoming increasingly resistant to these anti-microbial agents. Research and mechanisms are being following to prevent a strong resurgence of this disease.
STDs: Non-Gonococcal Infections
Non-gonococcal infections have been increasing in cases compared to gonococcal infections. The most common of these infections (and currently the most common STD overall) is chlamydia, which is caused by the microbe Chlamydia trachomatis. Unlike gonorrhea, females carry heavier symptoms of this disease compared to males. However, similar to gonorrhea symptoms, salpingitis, ectopic pregnancies, and pelvic inflammatory diseases can occur as a result of contracting this STD.
Additional non-gonococcal infections can be caused by strains of Mycoplasma hominid, coliform, streptococci, and staphylococci. The pathology behind these infections are different from gonococcal, where the infectious organisms are able to penetrate through the fallopian tube walls. This allows for blood-borne infections to overtake the body, beginning with the meninges and joint spaces, but can eventually enter the heart valves. As microbes, antibiotics are the common treatment options, which poses a risk for eventual antibiotic resistance. Vaccinations, such as for C. trachomatis, have been a topic for development.
Pelvic Inflammatory Disease
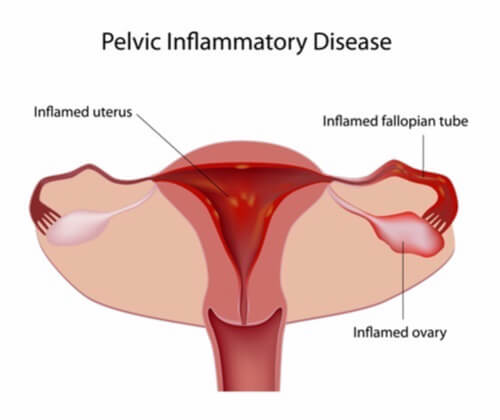
Pelvic inflammatory disease is an infection that occurs in the female reproduction system. It occurs when infections- typically STDs- spread from the reproductive tract and into the peritoneal cavity. Women may not experience any systems, but when symptoms are present, they include abdominal pain, bleeding when not menstruating, pain and bleeding during sexual intercourse, discharge from the vagina, and a burning sensation while urinating. If not treated early, pelvic inflammatory disease can lead to tissue scarring and blockages in the fallopian tubes, as well as increased chances of ectopic pregnancies and infertility. It is possible to cure this disease if it is caught early on, where treatments first look to remove the infection that led to the pelvic inflammation.
Cancers
Fallopian tube cancer is not as common as ovarian cancers, but they can still occur as either serous or endometroid in histology type. Out of the cancers that occur in the female genital tract, fallopian tube cancer makes up less than 2% of malignancies. However, data has shown that women who possess the BRCA mutation are at a higher risk of developing these adenocarcinomas, with most malignancies occurring specifically in the fimbria. BRCA is a gene that codes for a tumor suppressor, where mutations in tumor suppressor genes can increase the chances of developing cancer. This is a common mutation in both breast and ovarian cancers.

Because a correlation between fallopian tube cancer and ovarian cancer has been found, it is hypothesized that ovarian serous cancers may initiate within the fallopian tube. However, more research is needed to support this hypothesis. Treatments when fallopian tube cancer occurs- as well as cancers of the ovaries and uterus- include removal of the fallopian tubes.
Conclusions
The fallopian tubes are hollow ducts in the female reproduction system that stem from the uterus and indirectly connect with the right and left ovaries. They are responsible for accepting released oocytes and hosting the fertilization process if sperm is present. The luteal phase of the ovarian cycle primarily occurs in the fallopian tubes. As a prominent structure in reproduction, diseases and disorders found here can quickly become serious, with infertility being a potential result. Alternatively, the fallopian tubes offer a convenient location for permanent sterilization in women who do not wish to become pregnant.
Quiz
