Definition
The coronary sinus is a large vein located in the atrioventricular groove (coronary sulcus) between the left ventricle and atrium of the heart. This vein collects deoxygenated blood from several cardiac veins located around the heart muscle. At its origin, the coronary sinus drains into the right atrium. The coronary sinus ends at its junction with the great cardiac vein.
Coronary Sinus Location
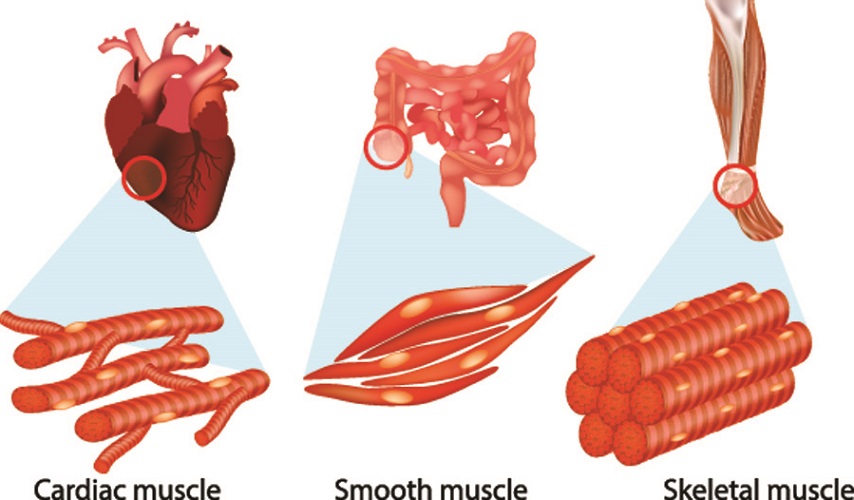
Studying the location of the coronary sinus requires basic knowledge of heart muscle and its surrounding blood vessels.
The heart muscle provides the pumping power of the heart and is unlike smooth and skeletal muscle tissue. Heart muscle tissue is also referred to as cardiac muscle or myocardium. The myocardium lies between the outer sac that covers the heart (epicardium) and the inner membrane (endocardium). Heart muscle also contains pacemaker cells that take over the role of neurons and initiate and transmit the action potentials that cause heartbeats.
All myocardium cells have large quantities of mitochondria to ensure consistent energy supply. Unlike other types of muscle, if the heart stops even for a very short period the results can be fatal. Heart muscle contractions occur in wave-like motions that propel blood in the right direction, from the top of the atria to the bottom, and through the ventricles to ensure enough blood is pushed into the aorta and pulmonary artery.
To ensure a supply of nutrients and oxygen, the myocardium is fed by coronary arteries. Deoxygenated blood and waste products are transported from the heart muscle via numerous coronary veins. These veins channel blood into the right atrium where it can join the pulmonary circulation. There are twice as many coronary veins as there are arteries – this is because veins also act as a reservoir system that can adjust blood flow into the heart. A ready supply of blood must always be available to fill the right and left atria.
Many of the coronary veins drain into the coronary sinus. The diameter of this vein and its proximity to the right atrium also make it an access point for various cardiac procedures such as ablation (for heart arrhythmia).
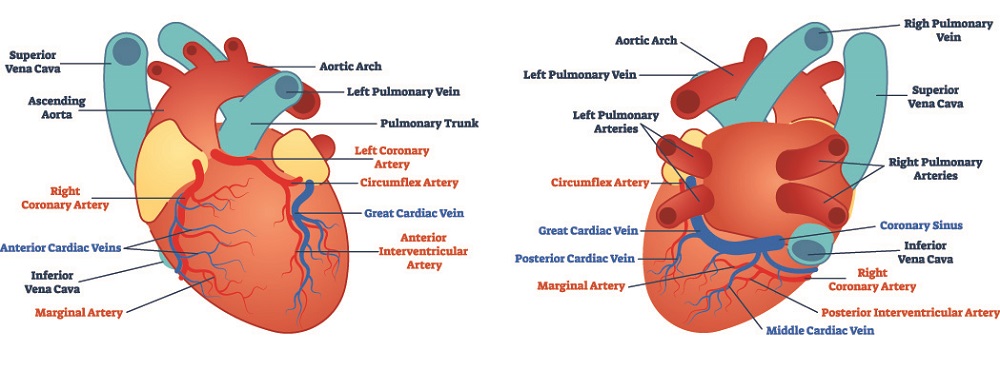
Two groups of veins drain deoxygenated blood from the myocardium – greater and smaller. The coronary sinus is part of the greater venous group, accepting blood flow from the great cardiac vein, small cardiac vein, inferior left ventricular vein, atrial veins, and middle cardiac vein.
The smaller cardiac vein group is comprised of Thebesian veins that empty directly into the chambers of the heart.
The coronary sinus is approximately two to five centimeters in length with a variable diameter of around one centimeter. This makes it the widest cardiac vein. It is located between the left atrium and ventricle, within the atrioventricular groove of the heart muscle that points towards the diaphragm (diaphragmatic surface). In the Gray’s Anatomy image below, the groove between the left atrium and ventricle is hidden behind the pulmonary artery and aorta. The visible groove between the right atrium and ventricle indicates this groove’s or sulcus’ appearance and position.

Coronary Sinus Function
Coronary sinus function depends on heart contraction – when the atria contract (atrial systole), the sinus also contracts. This is because its wall contains cardiac muscle cells in direct contact with the cardiac muscle of the atria.
Blood Reservoir
When this vein contracts, it pushes collected blood into the right atrium. With both contracting simultaneously and with the valve between the atria and ventricles open, more blood can pour into the right ventricle; however, most blood that enters the right-hand side of the heart is provided by the venae cavae.
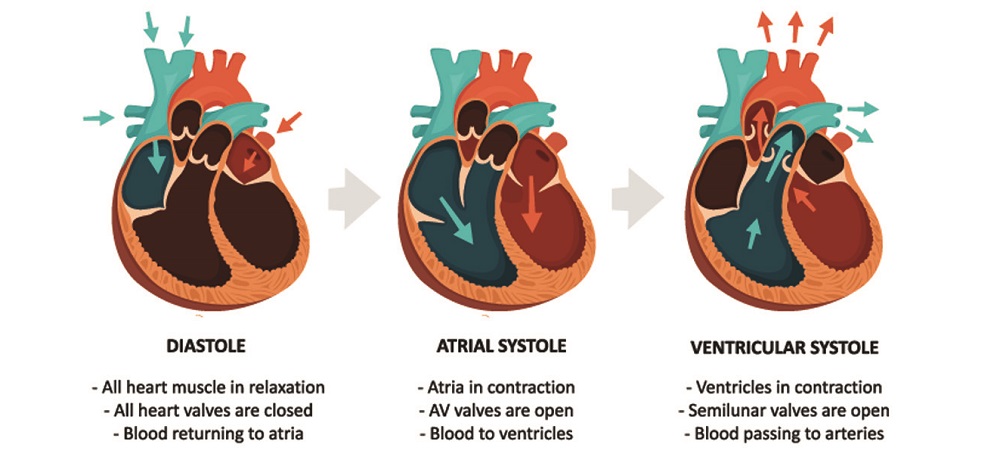
Coronary sinus anatomy includes valves that prevent blood from flowing in the wrong direction. Between the inferior vena cava and the tricuspid valve that stops blood from regurgitating from the right ventricle into the right atrium is the opening that marks the start of the coronary sinus. This opening is called the ostium and is partially covered by the Thebesian valve.
The end of the coronary sinus is marked by the valve of Vieussen’s that prevents blood from regurgitating back into the great cardiac vein.
Important to remember is that although it is located between the left atrium and ventricle, the coronary sinus opens into the right atrium; coronary sinus valves are found at the ostium and its connection with the great cardiac vein.
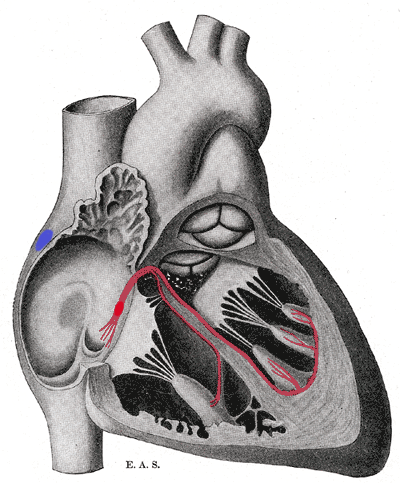
Nothing has been labeled in the below image – the blue spot shows the area where the sinoatrial node is located on the inside of the myocardium; the bundle of His is indicated in red.
Where the bundle of His originates, close to the inferior vena cava, you can see a crescent-shape guarding an opening. This opening is the ostium – the crescent is the Thebesian valve.
Drainage Point
The coronary sinus drains blood from various coronary veins. These veins collect deoxygenated blood from different areas of the myocardium.
The great cardiac vein, the lateral marginal veins, and the inferior veins all receive deoxygenated blood from the left ventricle. The middle cardiac vein or inferior interventricular vein drains venous blood from the myocardium surface. This vein eventually becomes the great cardiac vein.
The oblique vein of the left atrium (Marshall’s vein) transports deoxygenated blood from the left atrium. Finally, the small cardiac vein brings blood from the right atrium and part of the right ventricle. Other myocardium veins drain directly into the heart chambers.
Impulse Transmission
The coronary sinus has an electrical function as it also connects the right and left atrium. Because of this, it may even contribute to cases of atrial arrhythmia. As other large veins such as the superior vena cava and pulmonary veins are also able to trigger this disorder, this is no surprise. Small quantities of heart muscle cells connect directly to the larger veins of the heart and can provide additional stimuli for atrial contractions that have the potential to cause or encourage an irregular heartbeat or even atrial fibrillation.
The electrocardiogram (ECG) below shows an electrical fault inside the atria. A normal ECG has a P wave, QRS complex, and T wave. In the below example, the P wave is not composed of a single curve (atrial systole) but multiple, uneven waves. This shows that the electrical impulses that initiate atrial systole are not synchronized; impulses could be coming from various areas of the atrium, and not just from the sinoatrial node. Some of these abnormal impulses may be sent or transmitted via heart muscle cells in the sinus wall.

Coronary Sinus Pathology
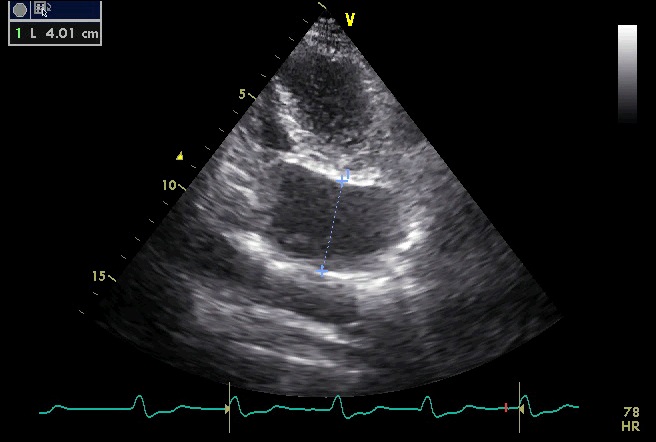
Heart pathology can be congenital or appear over time. As a vein, there is no formation of fatty deposits (atherosclerosis) in the coronary sinus; however, dilation due to arterial hypertension can occur. A giant coronary sinus of 4.5 centimeters in diameter has been recorded.
Unroofed Coronary Sinus Defect
Atrial septal defects (ASDs) are sometimes referred to as holes in the heart. An ASD occurs where an opening in the wall (septum) between the right and left atria remains open after birth. Usually, this opening closes either just before or shortly after birth. The opening is called the foramen ovale.
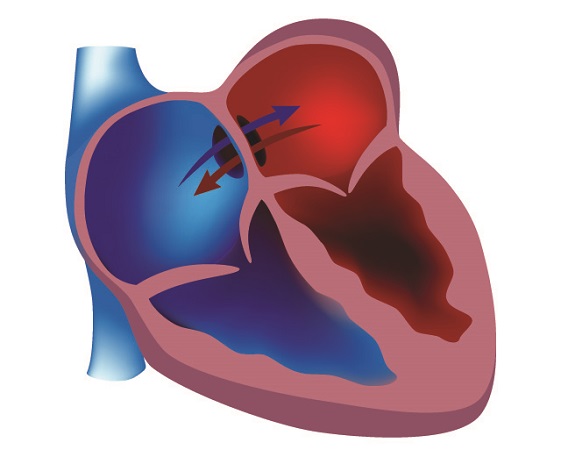
An atrial septal defect means that the foramen ovale does not close completely or at all; deoxygenated blood from the right atrium can flow into the oxygenated blood of the left atrium and vice versa.
A coronary sinus atrial defect is not a true form of ASD. The hole, in this case, is not in the septum but between the (unroofed) coronary sinus and left atrium. This gap can extend from the right to the left atrium, meaning deoxygenated and oxygenated blood can mix. This pathology gives similar symptoms to ASD.
Coronary sinus ASD only exists if the foramen ovale in the septum has not closed and the wall between the sinus and atria is not intact. Without a fault in the foramen ovale, this defect is referred to as an unroofed sinus.
With symptoms that seem much like those of an ASD, an unroofed coronary sinus defect (UCSD) is nearly always congenital and extremely rare. Symptoms include shortness of breath, swelling in the limbs and abdomen (edema), fatigue, and heart palpitations. If the defect is small, these symptoms may be absent.
Diagnosis of UCSD and ASD is via echocardiogram, electrocardiogram, MRI, and/or CT. Earlier diagnostic methods often confused an unroofed coronary sinus defect with ASD.

Coronary Sinus Arrhythmia
As the sinus wall also contains cardiac muscle cells, coronary sinus arrhythmia is another potential pathology. Either the presence of cardiac muscle in or very close to the sinus transmits impulses, or pressure due to a dilated coronary sinus (see next heading) affects the electrical pathways of the right atrium. The most common treatment type is ablation therapy where the areas that instigate action potentials outside of the sinoatrial node are cauterized.
Coronary Sinus Dilation
Coronary vein dilation is often a sign of ischemic heart failure and/or dilated cardiomyopathy (an enlarged and overworked left ventricle). A dilated vein is nearly always the result of increased blood flow.
In the coronary sinus, increased blood flow is primarily due to higher volumes coming into the heart through the venae cavae or to regurgitation from the right ventricle to the right atrium via a faulty tricuspid valve. This stops the sinus from draining properly and places pressure on its elastic walls. Just like a balloon, when blown beyond a certain level the vein will not be able to return to its original shape – it remains dilated and cannot contract as strongly as before.
Upon diagnosis of a dilated coronary sinus, a cardiologist will automatically suspect a problem with the right ventricle.
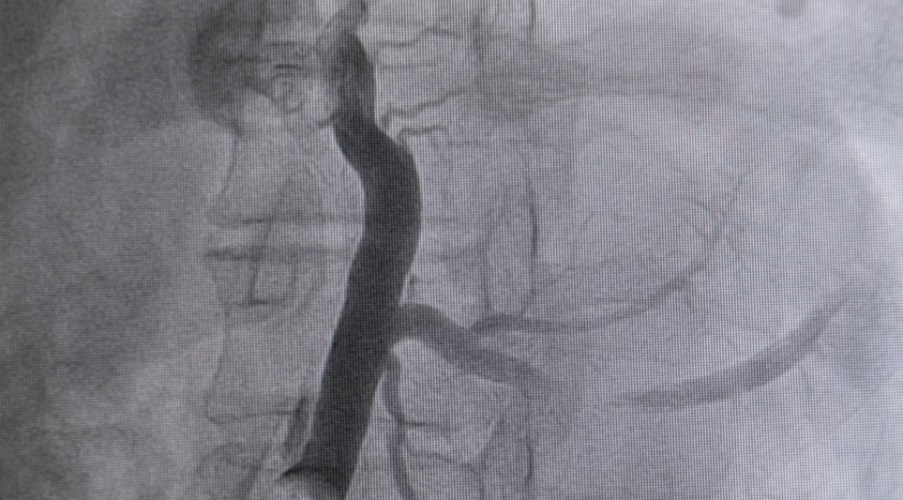
Measuring the diameter of the vein (below image) can indicate whether surgery is required.
Coronary Sinus Diverticulum
Another disorder is the diverticulum – a bulge in the vessel wall that weakens the vein and gradually causes dilation along its length. There is a risk that the weakened wall can leak, although coronary veins do not need to deal with the high pressures of the arteries closest to the heart and this is an extremely rare occurrence. However, when dilated the muscular walls of the coronary sinus are unable to contract or provide an efficient reservoir function.
The greatest risk with this pathology is blood clot formation. The normally smooth walls inside the vein allow blood to stream through it unhindered. When the vessel wall bulges outwards, the change in shape creates turbulence. Turbulence may lead to the formation of small blood clots. These are transported from the coronary sinus into the right atrium where the clots then travel through the right ventricle and straight into the lungs via the pulmonary artery. Blood clots can become stuck in the arterioles and capillaries of the lungs, blocking off blood flow with often serious consequences (pulmonary embolism).
Quiz
