Definition
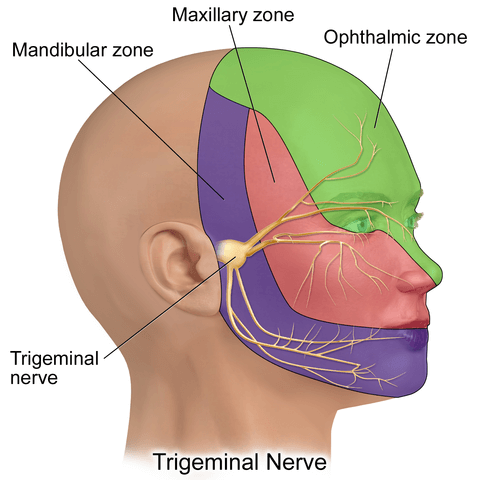
The trigeminal nerve is the largest cranial nerve (CN V); it transmits sensory information from the scalp, face, eye orbit, paranasal sinuses, and part of the tongue, and also plays a motor role for the mastication and facial expression muscles. With both sensory and motor components, the trigeminal nerve is a mixed nerve that splits into three divisions: the ophthalmic, maxillary, and mandibular branches.
Trigeminal Nerve Function
Trigeminal nerve function is also split into these three divisions or branches as each has its own roles. The ophthalmic nerve branch, or CN V1, the maxillary branch (CN V2), and the mandibular nerve branch, hardly surprisingly called CN V3 all do different things.
The trigeminal nerve originates from four nuclei or groups of CNS nerve cells that begin at the midbrain and end at the medulla oblongata. Three of these nuclei are sensory (the mesencephalic, principal sensory, and spinal nuclei). The fourth is known as the motor nucleus and sends out nerves that help with jaw movement. Everything you feel on and in your face, the front of your scalp, and the mucous membranes of your mouth, nose, and sinuses is due to the different branches of the trigeminal nerve.
The image below shows the thick trigeminal nerve ganglion at the end of the main trunk of the trigeminal nerve, just in front of the outer ear. It is from the trigeminal ganglion that the three branches or divisions begin. The branches (yellow) and the areas which these branches serve are also depicted – the ophthalmic (green), maxillary (pink), and mandibular (purple) zones.
CN V1 Function
Ophthalmic branch function is sensory (afferent) – afferent in this case means that sensory stimuli are sent towards the trigeminal nerve. The ophthalmic branch nerve is the smallest of the three branches but plays a substantial role.
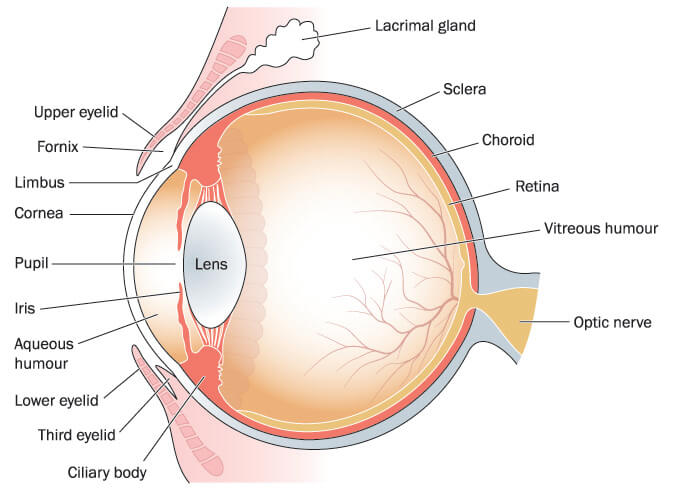
The sensory characteristics of CN V1 are responsible for sensory input from the cornea, iris, ciliary body, lacrimal gland, and conjunctiva. This branch also connects areas of the mucous membranes of the nasal cavity and the sphenoidal and frontal sinuses. The skin of the eyelids, eyebrows, forehead, and nose are also connected to CN V1. Finally, the ophthalmic branch of the trigeminal nerve serves the membranes that surround the brain and separate the cerebellum from the cerebrum.
The ophthalmic branch begins at the trigeminal ganglion – just like all of the trigeminal branches – and eventually divides into three smaller nerves known as the lacrimal nerve, frontal nerve, and nasociliary nerve. Knowing the names of these smaller branches is not necessary, but as they have specific functions it is worth listing them accordingly.
The lacrimal nerve innervates the lacrimal gland, upper eyelid, and conjunctiva. The frontal nerve further splits into supraorbital and supratrochlear branches; the first of these innervates the upper eyelid, conjunctiva, and scalp; the latter the upper eyelid, conjunctiva, and forehead. The nasociliary nerve divides into four divisions – they provide sensory innervation of the mucous membranes in the sinuses and nose. Finally, the long nasociliary nerve sends sensory information to the brain from the iris, cornea, and ciliary bodies that control the shape of the eye lens (see image below). Although some sources say the ophthalmic nerve dilates the pupils and produces tears, it is other nerve fibers that travel alongside CN V1 that perform these functions.
CN V2 Function
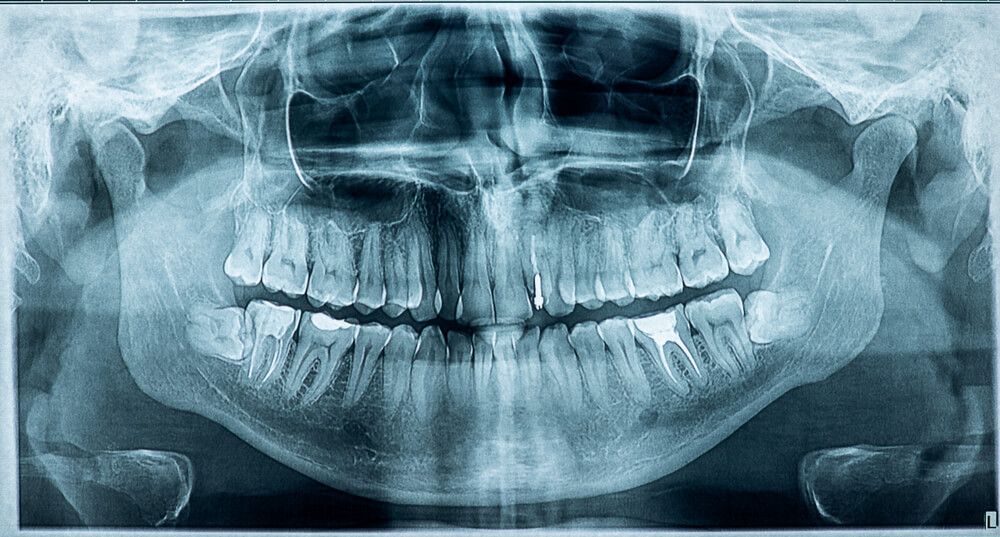
The maxillary branch (CN V2) enables sensation in the mid-region of the face (nasal cavity, sinuses, and maxilla). It has four divisions and these divisions also split so the entire face, as well as the membranes of the brain, are well innervated and extremely sensitive. For example, the superior alveolar nerves ensure we feel the uncomfortable pain of toothache when the teeth in the upper jaw become infected.
CN V3 Function
The mandibular nerve or CN V3 is a mixed nerve composed of efferent motor fibers and afferent sensory fibers that innervate the lower face, upper neck, oral cavity mucosa, and the gums and teeth of the lower jaw. This branch also splits, for example, into the inferior alveolar nerves that innervate the teeth of the lower jaw and, unlike the superior alveolar nerve, it also has motor fibers.
Mastication or the chewing of food involves using the powerful muscles that envelop the mandible and maxilla. Damage to this area of the trigeminal nerve can give a strange sensation when eating and completely change how we chew our food.
An example of trigeminal nerve function in the mandible is the innervation of the lateral pterygoid muscle by one of the motor branches of the mandibular branch. You can test this nerve by moving your lower jaw forward to produce an underbite, or open your mouth only by dropping the bottom jaw. This motor nerve also allows you to move your jaw from side to side. Another trigeminal nerve function example is the sensory buccal nerve branch of the mandibular nerve that allows us to feel a sensation on the cheek.

Trigeminal Neuralgia
Trigeminal neuralgia is trigeminal nerve pain and can be a debilitating disorder. Other names sometimes used to describe trigeminal neuralgia are tic douloureax or painful tic. This pain comes and goes, probably in reaction to inflammatory processes within the body, a low blood supply, nerve damage, or direct pressure to the nerve. Many neurological departments allocate specific teams for the diagnosis and treatment of trigeminal neuralgia patients.
Trigeminal neuralgia occurs more commonly in females over the age of 50. Symptoms begin suddenly and are usually short-lived and on one side of the face. Pain can be triggered when chewing, brushing the teeth, talking, or even when the face is gently touched or exposed to cold weather. The trigeminal branches most affected by trigeminal neuralgia are CN V2 and CN V3.

Other pathologies such as Herpes zoster, migraine, multiple sclerosis, and Tolosa-Hunt syndrome can also present with facial pain symptoms. Trigeminal nerve pain is then called secondary trigeminal neuralgia. Idiopathic trigeminal neuralgia is a form that presents with all the symptoms but does not have a detectable cause.
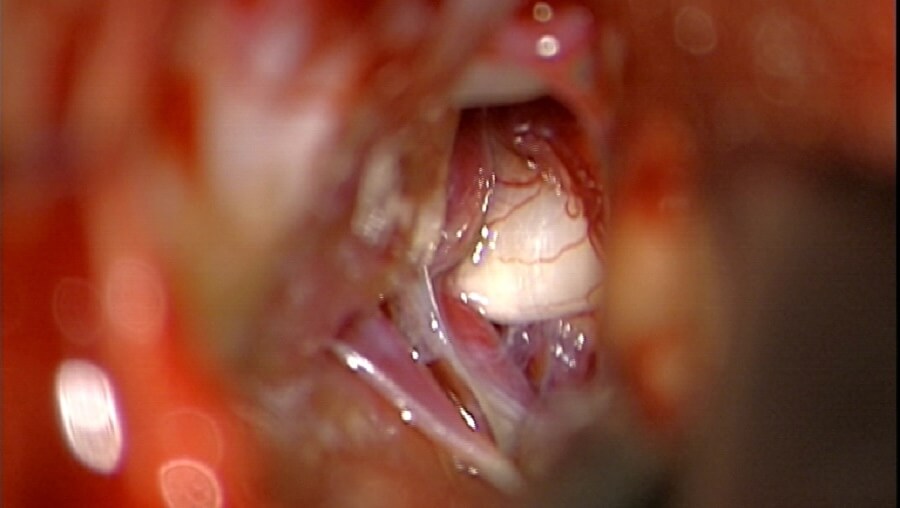
There are plenty of potential causes of trigeminal pain, but the easiest to diagnose is blood vessel pressure directly on the trigeminal nerve. Blood vessels lie incredibly close to the nerves; if they push into or wrap around a nerve they can form what is known as a neurovascular loop. Other causes directly related to the nerves are damage to the myelin sheath of nerve fibers and (surgical) trauma; however, the majority of cases are idiopathic – we just don’t know why.
Conservative treatment might be the injection of local anesthetics or Botox, and pharmaceuticals in the form of painkillers and anticonvulsants (carbamazepine) that stop blood vessel spasms that may cause a temporary reduction in blood supply to the nerve.
Surgical treatment of trigeminal neuralgia is a complex decompression procedure and not without risk. Surgeons must locate the site of a neurovascular loop or an area of compression and carefully unwrap or free the nerve from the tissues or vessels that provide pressure. These procedures can take many hours to perform and do not guarantee results. Some forms of trigeminal neuralgia have been successfully treated with stereotactic radiosurgery (gamma knife or CyberKnife) that is usually used to treat brain tumors. Unfortunately, however, this form of facial pain remains hard to treat and extremely difficult to cure.

Quiz
