Definition
Junctional rhythm describes a heart-pacing fault where the electrical activity that initiates heart muscle contraction starts in the wrong region. Heart rhythm is the result of electrical impulses sent from the pacemaker cells of the sinoatrial node (SAN) at the top of the right atrium. If the SAN fails to fire, an area located at the meeting point of the atria and ventricles (atrioventricular junction) takes over the role of pacemaker, causing junctional rhythm.
Junctional Rhythm vs Sinus Rhythm
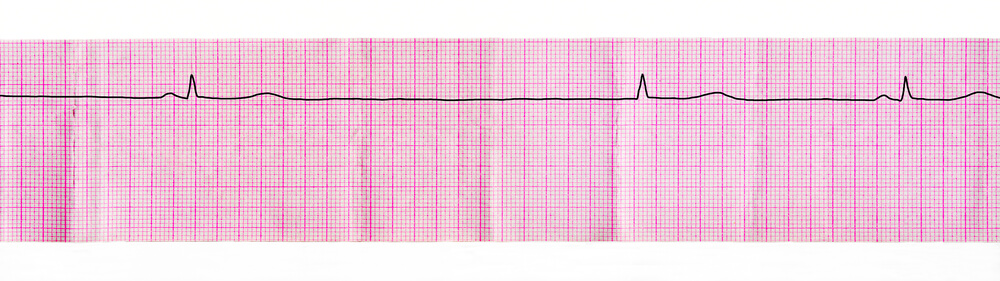
Junctional rhythm and sinus rhythm have almost the same result – both types send electrical impulses through specialized heart muscle (cardiac muscle) to force certain areas of the heart to contract at certain times. In which order these muscles contract is extremely important – from the top to the bottom of the atria, a tiny pause, and then across the ventricles. This forces blood to be pumped through the chambers and into the lungs or the rest of the body. You will probably have come across the image below before – the famous circulatory system that sends nutrient and oxygen-rich blood into our tissues or collects waste products and sends them to the liver and urinary system. How slowly, rapidly, or efficiently our hearts contract is integral to our overall levels of health.
In a healthy heart, the sinoatrial node (SAN) is the default pacemaker. What does a pacemaker do? It’s a good idea to imagine an army drum that tells soldiers when to take a step. If the drum beats quickly the soldiers make a lot of ground – the heart pumps as much oxygen around the body as it can. When the heart slows the soldiers probably won’t reach their destination on time; the heart might not receive enough oxygen. This is why your heart beats faster when exercising. The location of the sinoatrial node or SAN is at the top of the right atrium in an area of tissue called the triangle of Koch. The sinoatrial node is not an easy to distinguish structure – it looks the same as any other area inside the heart – and the only differences are seen under extreme magnification. You should think of the SAN as an area of specialized pacemaker cells.
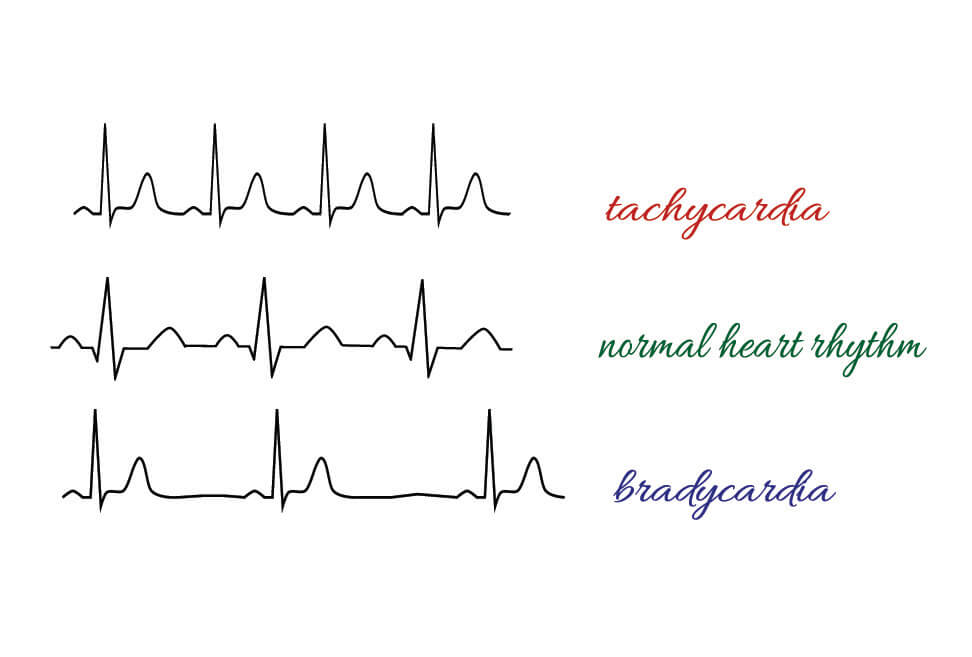
Sinus rhythm describes the normal electrical activity of the heart that allows the heart muscle to contract (myocardial contraction). All muscle contraction, whether cardiac, skeletal, or smooth, depends upon action potentials. These are electrical impulses that cause individual muscle fibers to contract. Where the heart is concerned, contraction of the heart chambers allows blood to be pumped around the body. Normal sinus rhythm (NSR) originates at the sinoatrial node at an average rate of 60 to 100 beats per minute (bpm). If you feel your pulse, chances are you will feel a sinus rhythm. If your heart beats faster than 100 bpm this is known as sinus tachycardia; rates below the normal range are known as sinus bradycardia. The term heart rate is synonymous with the rate of pacemaker depolarization.
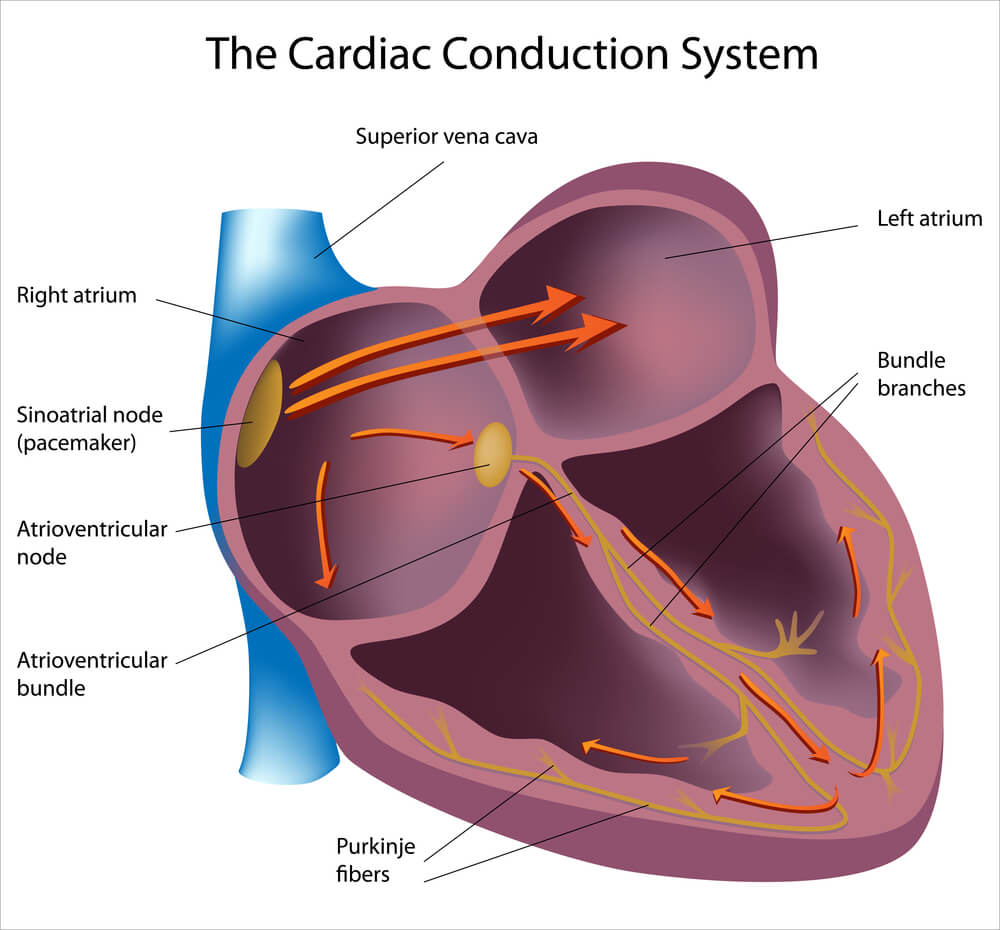
Junctional rhythm is not the same as a sinus rhythm. This is because the place where pacing takes place (the drum section) moves to another area known as the atrioventricular junction. In junctional rhythm, the atrioventricular junction becomes the default pacemaker and the resulting heart rate is then called a junctional rhythm, not a sinus rhythm. There is no difference to how these two areas function – they are both composed of pacemaker cells – but the target cells differ and this is an important difference. The SAN activates contraction in the atria while the AV junction does the same for the larger, more powerful ventricles.
When at rest, the cells of the heart muscle or myocardium are polarized – electrical charges on either side of the cell membrane differ with a lower charge inside the cell. These cells that are found in the thick atrial and ventricular walls must wait for a slightly-charged stimulus so they can depolarize. This is a complex mechanism where charged ions pass through the cell membrane to create an electrical change.
However, some myocardial cell types do not need a stimulus to depolarize. These cells are called pacemaker cells. They are most commonly found in groups and it is these cells that create the conducting system or pacemaker system of the heart.
Most pacemaker cells are found in the area of tissue known as the sinoatrial node. Other, smaller groups are found at the atrioventricular node and in the bundle of His and Purkinje fibers that branch out from the heart septum and make their way through the left and right ventricles.
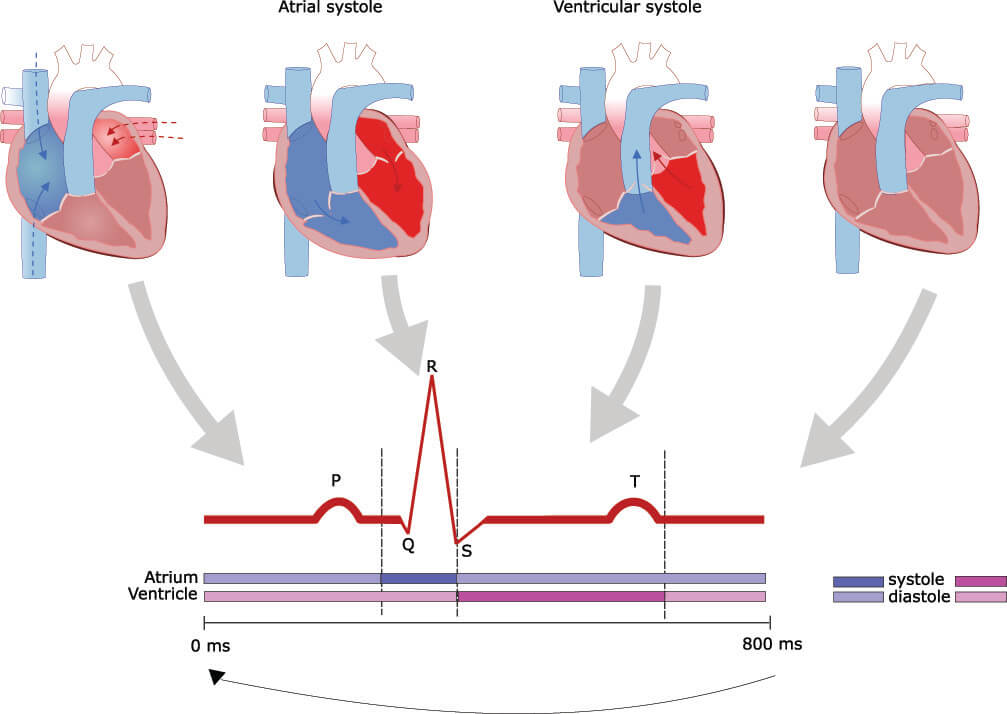
In a normal heart, the rate of depolarization of the AVN, bundle of His, and Purkinje fiber pacemaker cells is slower than the depolarization rate of the SAN. This is very important, as when the SAN fires more rapidly its signals are dominant and control the electrical activity of the heart. This means that electrical activity starts at the top of the atria and works its way down through the atrioventricular junction and then the bundle of His and Purkinje fibers. If the SAN fails to fire, or if neighboring cells fail to pass on the signal, the AV junction that continuously fires at a slower rate in the background – takes over. This is an extremely helpful mechanism. It means that if the sinoatrial pacemaker cells are permanently damaged it is still possible to have some heart activity. However, if you remember, the target cells of each node are different; the SAN targets the cells of the atria and the AVN the cells of the ventricles. This means that AVN pacing does not allow proper contraction of the two atria (systole) and will mean the heart functions less efficiently as the ventricles do not sufficiently fill with blood and less blood is pumped from the ventricles (diastole) into the rest of the body. The following image shows the association between electrical activity and heart muscle contraction.
Cardiac Rhythm on the Electrocardiogram
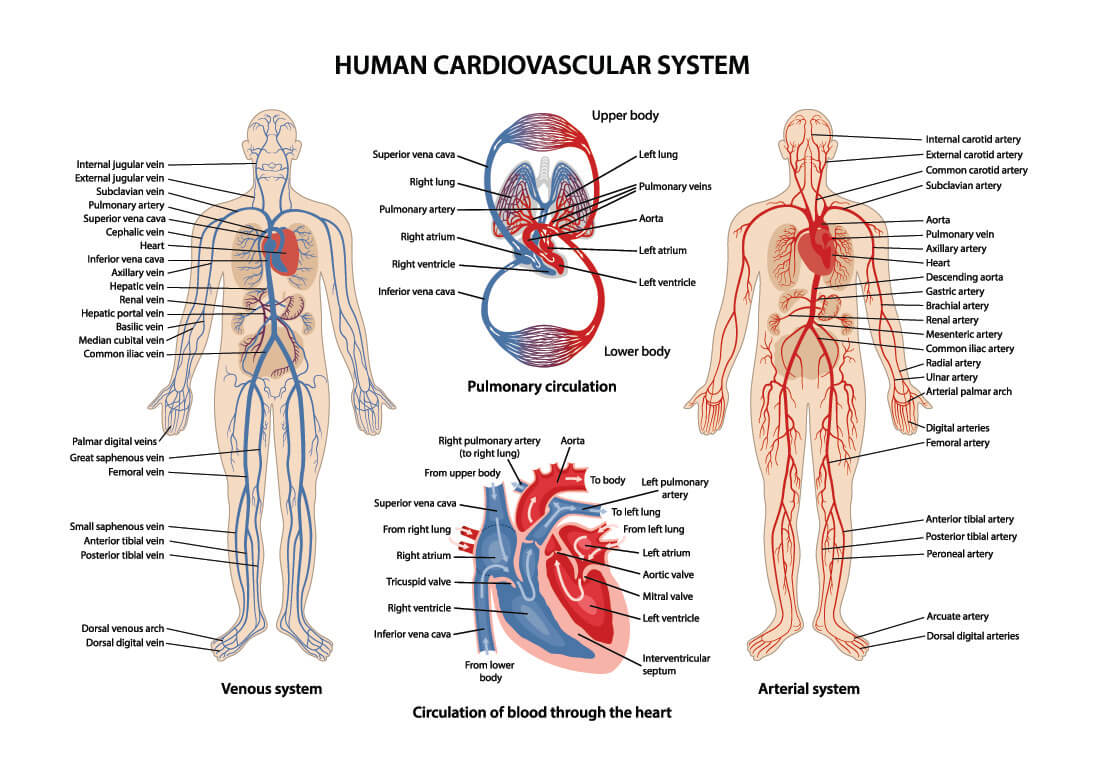
Cardiac rhythm can be observed by way of an electrocardiogram (ECG). You will have seen the ECG symbol on many medical business logos. Both heart rate and heart activity are measured on an electrocardiogram that maps most of the electrical activity of the heart but not all of it. The SAN is a very small area of tissue and its activity is not seen on an electrocardiogram. We can only figure out its function by looking at the depolarization of the right and left atria. When these larger areas of muscle tissue contract, the surge of electricity is shown on the ECG as the P wave.
The next step is a short pause between the P wave and the start of the QRS complex. This pause is controlled at the atrioventricular node, once impulses have arrived there from the SAN. The delay is not long – just a tenth of a second – but it is enough to give the ventricles time to fill with blood.
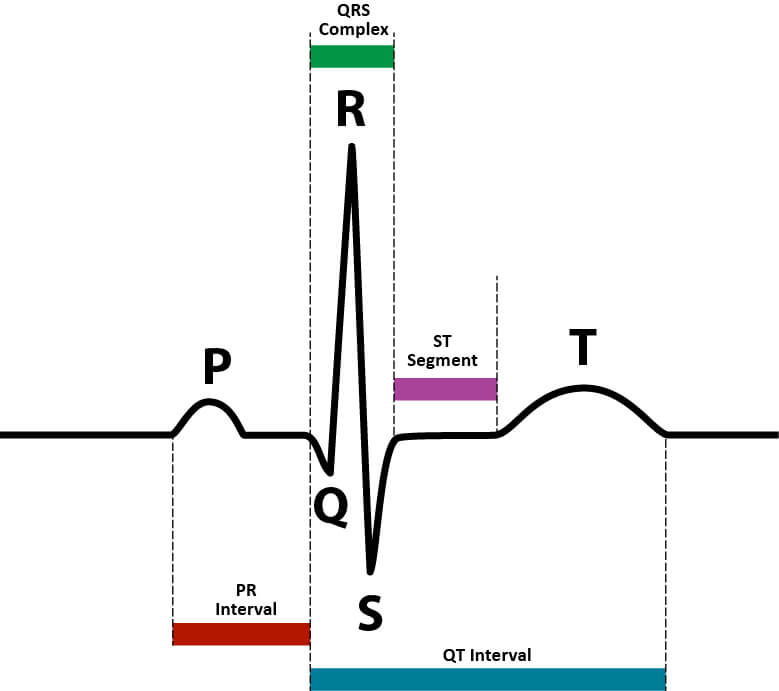
So if we know that the P wave is the result of atrial contraction caused by stimulation from the sinoatrial node, we should then find it easy to understand why, in junctional rhythm, the P wave is absent. Pacing only begins at the point where the pause before the QRS complex is found. In some cases, junctional rhythm might accompany an inverted P wave or retrograde P wave that shows depolarization leading back to the sinoatrial node from the AV junction. After all, the heart does everything it can to keep us alive and these escape pathways give a person an even greater chance of survival.
The QRS complex is the result of the firing of the AVN firing, usually under the pacing control of the SAN. This time, instead of the atrial walls, the ventricle walls depolarize. The width of the QRS complex shows how long it takes for the electrical signals to pass from the AVN, through the Purkinje fibers and along the walls of the left and right ventricles.
The final part of the ECG, the T wave, indicates ventricular repolarization. It is the gap between the T wave and the next P wave that changes our heart rate. A wider pause will produce a slower heart rate; a shorter pause a quicker heart one. You can see the difference in interval time between the T and P waves in the image below. Pacemaker cells – most commonly in the sinoatrial node – affect this gap; they fire prematurely (tachycardia) or a little later (bradycardia). In cases of bradycardia, there is a chance that the AVN will take over from the SAN as the AVN typically fires at a rate of 40 to 50 times per minute.
How rapidly the heart beats is not the decision of the pacemaker cells. They are reacting to our parasympathetic and sympathetic autonomic nervous systems. Parasympathetic activity uses acetylcholine to attach to the M2 muscarinic receptors of the pacemaker cells in the sinoatrial node to slow down the firing rate. Sympathetic activity releases noradrenaline that attaches to B1 adrenoreceptors on the same cells that make the pause between each heartbeat shorter, speeding up the heart rate. Receptors for acetylcholine and noradrenaline are found in both the SAN and at the AV junction and will affect the default pacemaker.
You might wonder why the heart doesn’t receive two orders to contract by both the SAN and the AVN. Well, the atria are extremely well insulated from the ventricles; this means that a signal from the sinoatrial node can’t make the ventricles contract without the assistance of the AVN. The AVN continues the chain of depolarization from the atria, through the bundle of His and into the ventricles. This is a lot more work than the sinoatrial node has to do (creating a larger wave on the ECG) and takes a little more time. The pause between SAN and AVN firing is therefore extremely important, as this allows the atria to empty via gravity and contraction, but also makes sure the ventricles have enough time to fill.
Types of Junctional Rhythm
The three types of junctional rhythm are categorized according to the resulting heart rate. In order of ascending beats per minute (bpm), these are junctional rhythm (or junctional escape rhythm), accelerated junctional rhythm, and junctional tachycardia.
Junctional Bradycardia
Junctional bradycardia is diagnosed when heart rates of below 40 bpm are the result of AV junction pacing. This may occur because the sinoatrial node is depolarizing too slowly, only working during occasional intervals or not working at all. These three causes are sometimes classified in the medical term sick sinus syndrome – a very broad description of all types of abnormal heart rhythms but most commonly bradycardia. Junctional bradycardia can also be the result of medication, a vasovagal reaction, hypothyroidism, and the mechanical disruption of a normal signal from the sinoatrial node that is called a sinoatrial block. Many other disorders can cause junctional bradycardia.
As the normal rate of the AV junction is 40 to 50 firings per minute, extreme bradycardia (40 bpm or less) will usually have more than one cause – with a faulty SAN that forces the AVN to take over we would expect heart rates of 40 to 50 bpm; anything less means something else is contributing to the slow heart rate. A slow heart rate is unable to supply the body with sufficient oxygenated blood. Symptoms are syncope, lightheadedness, and dizziness. Long-time (chronic) symptoms cause cell and tissue necrosis that affect the efficiency of every organ of the body.
Accelerated Junctional Rhythm
Accelerated junctional rhythm (AJR) describes a depolarization rate of between 60 and 100 per minute with heart pacing initiated at the AV junction. The most common cause of accelerated junctional rhythm is digoxin (digitalis) toxicity. Digitalis, or the foxglove, used to be one of cardiology’s most important plants but has now been nearly completely replaced by synthetic drugs.

Junctional Tachycardia
Junctional tachycardia occurs when the heart rate is over 100 beats per minute and the default pacemaker is the AV junction. This is a type of supraventricular tachycardia (SVT). This word simply describes a rapid heart rate that begins above (supra) the ventricles and can either be the result of rapid sinoatrial or atrioventricular node firing. SVT can last for minutes or hours and can be triggered by caffeine, alcohol, or drugs. Many people with SVT do not present with symptoms and aren’t even aware they have it. Most cases will not cause long-term problems but there is a chance SVT can evolve into more serious heart disorders.
Junctional tachycardia is also known as automatic or paroxysmal junctional tachycardia. We can describe it simply by saying it is a form of SVT where the over-rapid pacing of the AV junction overrides a slower rate of firing in the SAN. Accelerated junctional rhythm is usually seen in adults with heart disease or who are or have recently experienced acute myocardial infarction.
Junctional Rhythm Treatment
Junctional rhythm treatment does not treat the result (junctional rhythm) but the cause of the changed rate of depolarization. As we have already mentioned, pacing is controlled by the neurotransmitters acetylcholine and noradrenaline. Extreme bradycardia may require treatment with atropine which replaces parasympathetic acetylcholine in the muscarinic receptors of the pacemaker cells to force a sympathetic response – the heart rate speeds up. Atropine is derived from the belladonna plant or deadly nightshade. Adenosine is used to slow down the heart in cases of junctional rhythm SVT – often the heart will stop for one or two beats during this treatment and can give the patient an extremely uncomfortable feeling. Digitalis overdose requires treatment with both atropine and digoxin-specific antibody.

Where sick sinus syndrome is the cause of junctional rhythm, a permanent pacemaker should be fitted during a surgical procedure. These electrical devices take over the role of the SAN and/or AVN and send electrical impulses either constantly or take over if the heart fails to produce electrical stimuli itself. A battery is placed under the skin and electrical wires threaded into the right side of the heart and programmed to emit electrical impulses according to the patient’s pathology. Newer versions of pacemakers (nanopacemakers) do not need such a visible battery pack, as seen in the image below.
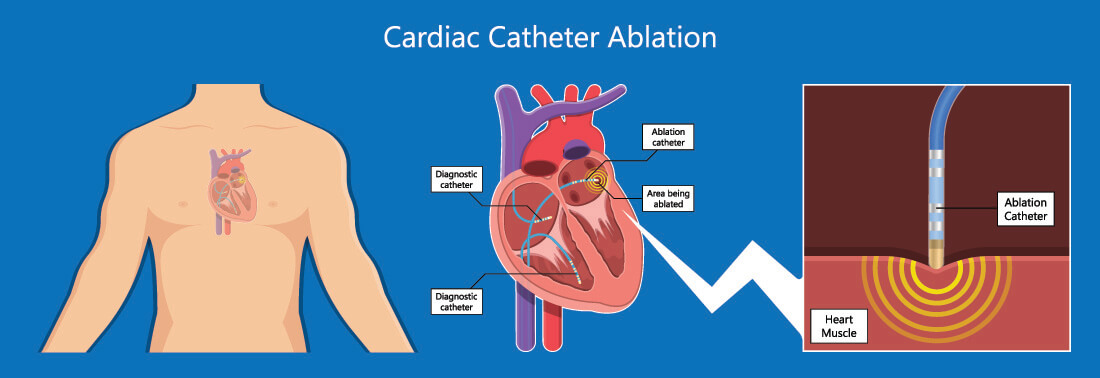
Babies with a persistent and symptomatic junctional tachycardia are treated with radiofrequency ablation; this may or may not be used as a treatment in adults. Ablation, in this case, involves the burning away of the areas of pacemaker cells close to or in the atrioventricular node that are responsible for the excessive firing. Once these have been removed, there is a greater chance that the sinoatrial node will become dominant again. In older adults, the cause may be sick sinus syndrome, and burning away AVN tissue may not make a difference or make the condition worse.
Many junctional rhythms are completely asymptomatic and only discovered during routine examinations. The majority of asymptomatic cases need no treatment.