Definition
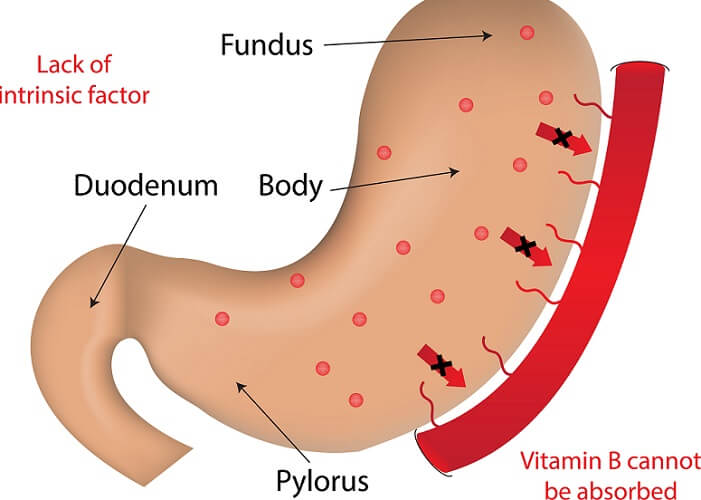
Intrinsic factor is produced by specialized mucosa cells called oxyntic cells located in the stomach lining. It is essential for the uptake of vitamin B12 at the end of the small intestine. This glycoprotein has two binding sites: one for binding B12 and one for a cell receptor that attaches to the bound intrinsic factor and B12. Failure to produce intrinsic factor affects red blood cell maturation and, therefore, causes a condition called pernicious (fatal) anemia. Thanks to vitamin B12 injections, this condition is unlikely to cause death today.
What is Intrinsic Factor?
Intrinsic factor (IF) is a glycoprotein secreted into the gastric juice. It has three synonyms:
- Gastric intrinsic factor (GIF)
- Cyanocobalamin (CO-60)
- Cobalt chloride (CO-60)
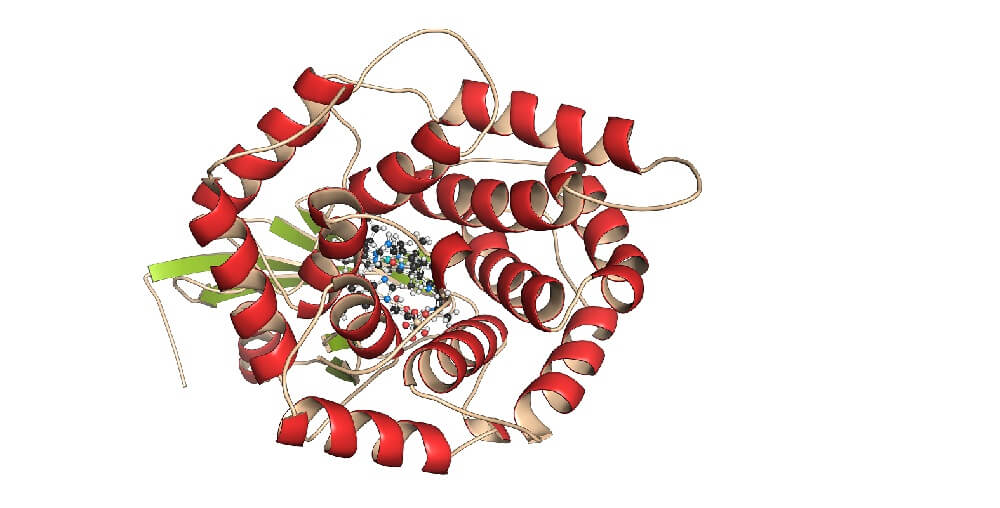
It is composed of carbohydrate (glyco) and protein. One molecule of intrinsic factor binds to one molecule of vitamin B12. Another name for this vitamin is cobalamin (Cbl). When intrinsic factor and cobalamin bind, the resulting molecule is referred to as IF-Cbl complex.
Intrinsic factor is secreted by parietal cells (oxyntic cells) of the stomach wall; in some smaller mammals it is synthesized in chief cells. Oxyntic cells secrete intrinsic factor as well as hydrochloric acid that makes the stomach contents very acidic. This is part of our natural immune barrier; high acidity destroys many of the bacteria we ingest.
Parietal cells are found in glands of the stomach lining, specifically the stomach fundus and cardia that lie close to the esophagus. These cells produce much more intrinsic factor than is needed. This means that problems in intrinsic factor production indicate more than 99% of the secreting capacity of oxyntic cells has been halted.

Vitamins and Intrinsic Factor
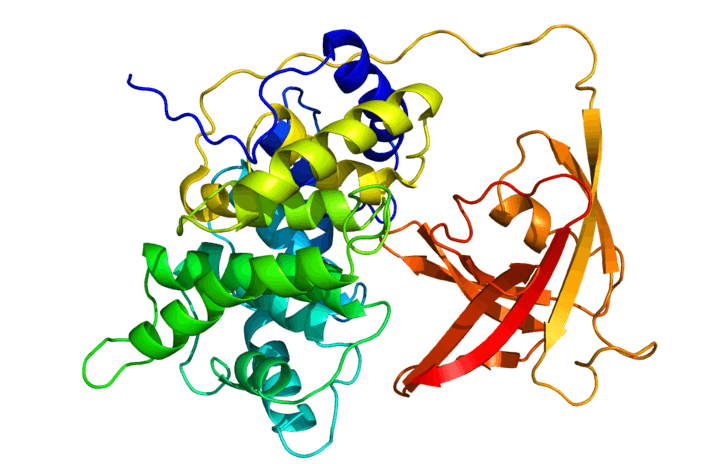
If you are asked, “which vitamin requires intrinsic factor in order to be absorbed?” there is only one answer: vitamin B12. Intrinsic factor function is singular – it contributes to the cobalamin journey. Three protein-based molecules are necessary for B12 uptake, transport, and storage:
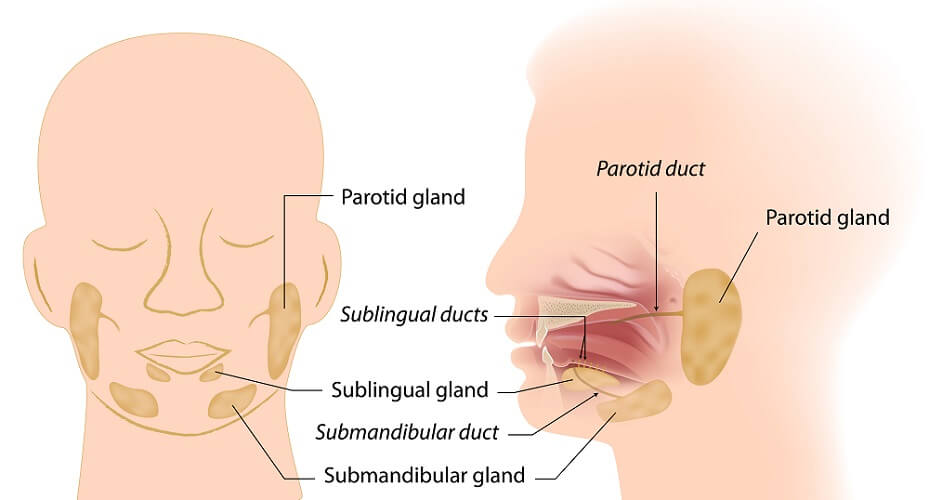
- Haptocorrin: synthesized in the salivary glands and bile
- Gastric intrinsic factor (GIF): synthesized in the upper stomach wall
- Trans-Cbl II: synthesized in the villi of the small intestine
Of these, only GIF and haptocorrin are glycoproteins; trans-Cbl II does not contain carbohydrate.
Vitamin B12 is not produced by the body and is an essential vitamin that enters the body via food. Sources are meat, fish, and dairy products. Today, most breakfast cereals are fortified with various vitamins and minerals including cobalamin. While the body does not synthesize this vitamin in its cells, it has now been shown that some gut bacteria can produce small quantities . Proven vitamin B12-producing bacteria species are Pseudomonas and Klebsiella. However, it is also said that these bacteria produce B12 analogs which cannot be synthesized in the same way as dietary sources; some may even interfere with dietary cobalamin uptake.

Another source of vitamin B12 outside of the foods we eat comes from the breakdown of tissues that contain it. This is why, unless there is a deficiency in B12 transport molecules, low levels of this vitamin may not cause symptoms until a decade or more later. Intrinsic factor deficiency or the presence of intrinsic factor antibody, however, causes symptoms such as anemia at a very early stage.
We need vitamin B12 for various physiological processes. The main intrinsic factor function is its role in red blood cell maturation. Other roles are DNA synthesis and nerve cell maintenance. These functions are achieved in combination with folate (vitamin B9).

Cobalamin Absorption
As cobalamin is found in high-protein foods, the acidic environment of the gastric juice first separates it from surrounding proteins.
The next step of cobalamin transportation is binding with haptocorrin. As we chew, saliva is produced that contains haptocorrin; this is carried to the stomach with food. Haptocorrin binds more than 50% of vitamin B12 in gastric juice and up to 80% of cobalamin in the blood plasma. When a haptocorrin molecule is bound to B12 it is referred to as holohaptocorrin.
These percentages show us that not all B12 moves immediately into the gut but much is taken, bound to haptocorrin, to the blood supply. The vitamin cannot be utilized until it has been freed and comes into contact with intrinsic factor in the ileum (small intestine).
In the low pH of the stomach, haptocorrin is much more likely to bind with vitamin B12 than intrinsic factor. Once in the blood, holohaptocorrin is taken to the liver and is transferred to the bile ducts and on into the duodenum. It is the constant movement of holohaptocorrin in the stomach, blood, liver, bile duct, gall bladder, duodenum, and small intestine that gives rise to the enterohepatic circulation of vitamin B12.
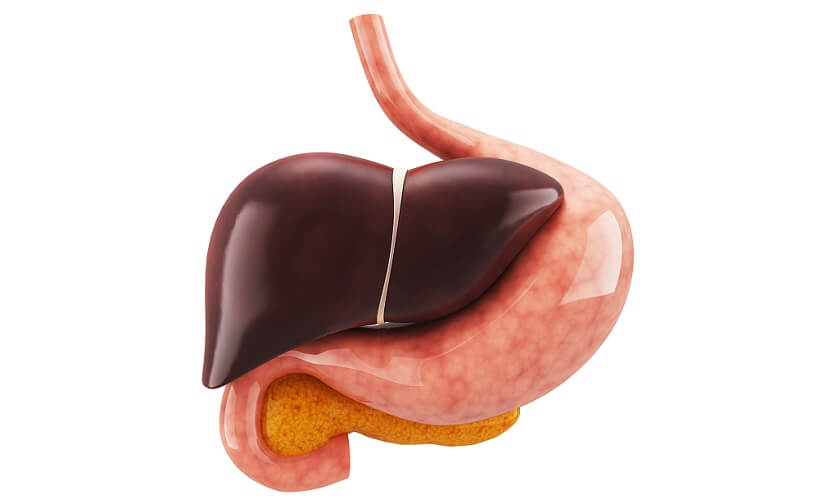
In order to be absorbed, intrinsic factor receptors must bind to separated molecules of vitamin B12. As these are bound to holohaptocorrin, another step needs to take place. This is the degradation of haptocorrin by enzymes produced in the pancreas. The pancreas empties pancreatic juice containing these enzymes into the duodenum. As the pH of the stomach contents becomes lower inside the ileum, the now-released vitamin is able to bind to intrinsic factor more easily. Together, they form intrinsic factor cobalamin complex (IF-Cbl). In simple terms, this is two conjoined B12/intrinsic factor molecules.
The availability of intrinsic factor plays a primary role in how much vitamin B12 is absorbed and used. If intrinsic factor levels are low, free cobalamin will simply exit the body via the feces. The amount of free B12 does not seem to influence intrinsic factor synthesis and IF is produced at a steady rate in healthy individuals.
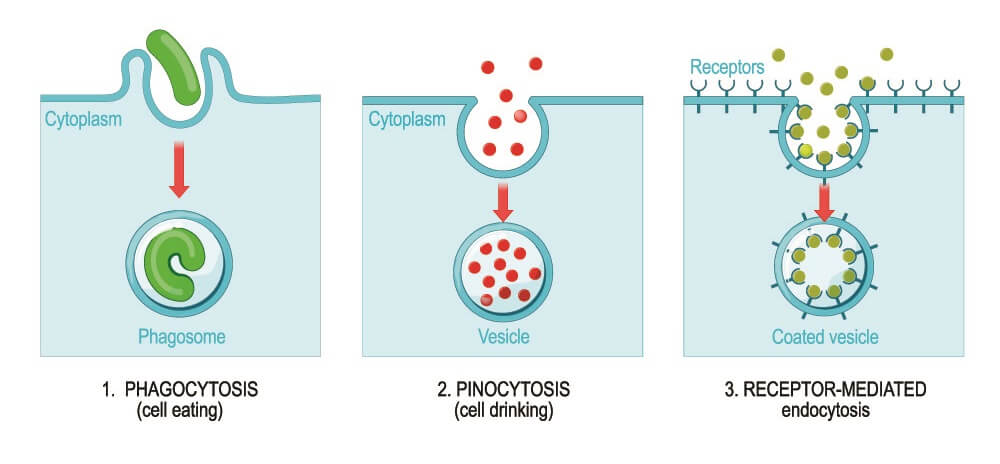
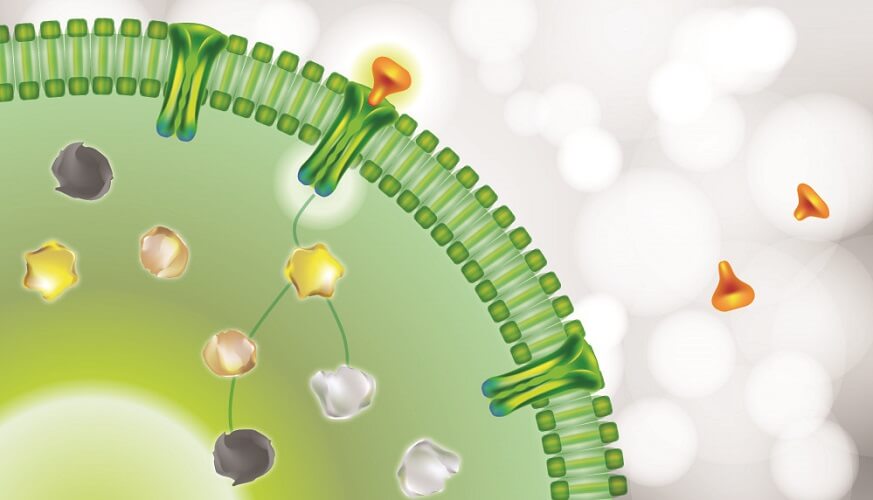
Once a molecule of IF-Cbl has been formed, the cells of the ileum wall can absorb it via receptor-mediated endocytosis (see image below). Here, cellular enzymes once more free the cobalamin – this time from intrinsic factor. This process allows trans-Cbl II to bind with and bring cobalamin to the bloodstream ready for use. This new complex enters the portal circulation: the portal veins bring blood from the digestive tract to the liver.
At any one time, trans-Cbl II transports up to 30% of cobalamin via the blood to those cells that can utilize it. These cells have receptors for saturated (cobalamin-carrying) trans-Cbl II. The complex enters the cell, cellular enzymes break it down, and the vitamin can finally play its various roles.
Intrinsic Factor Deficiency
Intrinsic factor deficiency stops the body from using vitamin B12 efficiently or at all, no matter how high the B12 levels are. In this case, oral cobalamin supplementation will have little effect. The only known and effective treatment for IF deficiency is intramuscular or intravenous injection of hydroxocobalamin. This molecule arrives in the liver, bypassing the intestine and skipping the steps of haptocorrin and intrinsic factor binding.

Intrinsic factor production can be reduced or halted by the intrinsic factor antibody. IF antibody prevents intrinsic factor from binding to cobalamin or stops cells from absorbing IF-Cbl complex.
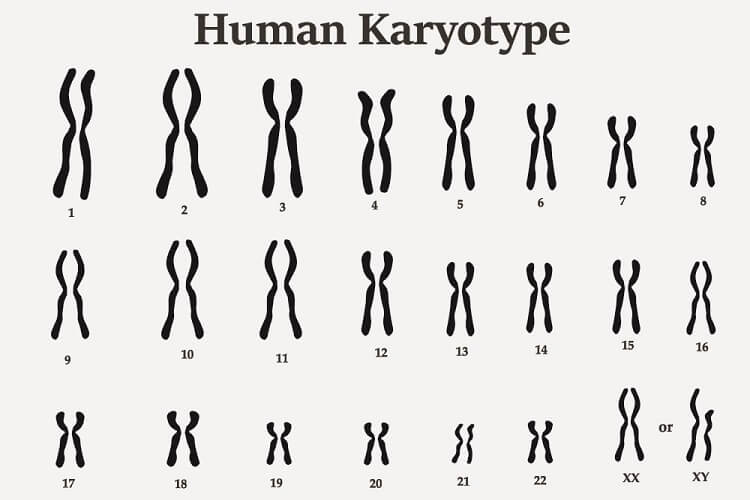
Gene expression for intrinsic factor synthesis is controlled by information in our DNA on chromosome number 11 – more specifically at chromosome location 11q12.1. If this GIF gene is damaged on both chromosome alleles, less or no intrinsic factor is produced.
Two types of intrinsic factor antibody tests can be carried out:
- Intrinsic factor blocking antibody type 1
- Intrinsic factor blocking antibody type 2 (also called precipitating antibody type 2)
Type one IF blocking antibody stops B12 from binding to IF in the ileum. Most cases of pernicious anemia are caused by this type of IF deficiency.
Type two IF blocking antibody prevents cells in the ileum lining from absorbing IF-Cbl complex molecules.
Intrinsic Factor and Pernicious Anemia
Pernicious anemia is the most common result of continuously low levels of vitamin B12. Symptoms include megaloblastic anemia (very large red blood cells in low numbers) and nervous system disorders such as vision problems, memory loss, and pins and needles. Other signs include fatigue, pale skin, and even psychosis. Up to the 1970s, pernicious anemia was common. As late as the 1950s, it was often a death sentence.
After the introduction of fortified foods in and around the 1970s, case numbers dropped significantly. Today, vegans are most susceptible to pernicious anemia; however, this is caused by low levels of dietary sources of vitamin B12 and not by an intrinsic factor disorder. Oral supplementation can rectify this.
Pernicious anemia in the presence of an omnivorous diet is either associated with intrinsic factor antibodies or genetic disorders.
With the production of intrinsic factor antibodies, parietal cells of the gastric lining are gradually destroyed leading to lower levels of IF. IF antibodies also block two different binding sites during the cobalamin journey.
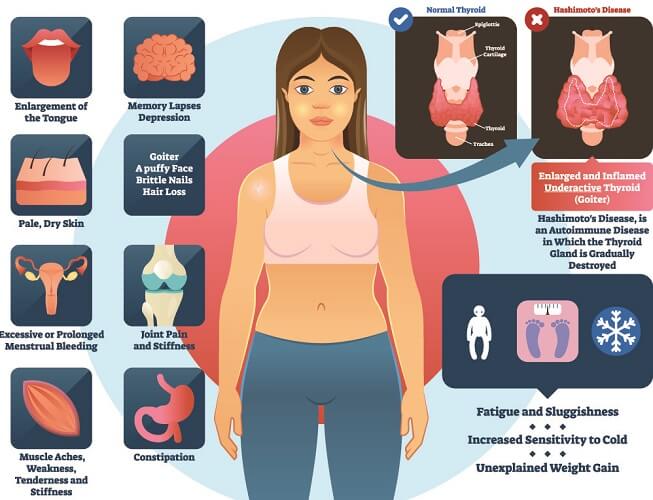
Various autoimmune diseases are linked to pernicious anemia. The most common are:
- Grave’s disease
- Hashimoto’s thyroiditis
- Insulin-dependent diabetes mellitus
- Myasthenia gravis
- Rheumatoid arthritis
Intrinsic factor deficiency syndrome is an extremely rare, congenital disease caused by autosomal recessive inheritance. Symptoms are commonly present by the age of five years. As with all forms of IF deficiency, anemia and nervous system symptoms are present. Children and sometimes adults (after mutation or the triggering of abnormal responses in their DNA) have mutations on both alleles of the gastric intrinsic factor gene on chromosome 11.