Definition
The Glasgow Coma Scale is a medical scale designed to assess the depth (and duration) of impaired consciousness and coma states. It helps to measure acute and chronic brain impairment within a trauma scene or during hospitalization; it is also used to predict whether a victim or patient is likely to die (prediction of mortality).
What is the Glasgow Coma Scale?
Most medical staff know what the Glasgow Coma Scale is and have been specifically trained to use it. Even though non-medical staff might find this scale helpful on the scene of an accident, it is much more important that they work according to the ABC of emergency care – Airway, Breathing, and Circulation.

Named after the university in which it was developed by neurosurgeons Graham Teasdale and Bryan Jennett, the Glasgow Coma Scale (GCS) was first published in The Lancet in 1974. Only in the 1980s, when recommended in the first edition of Advanced Trauma and Life Support, did its use become common.
The scale is still used today; even though there are various modern Glasgow Coma Scale alternatives, the GCS is one of the quickest methods of determining brain function.
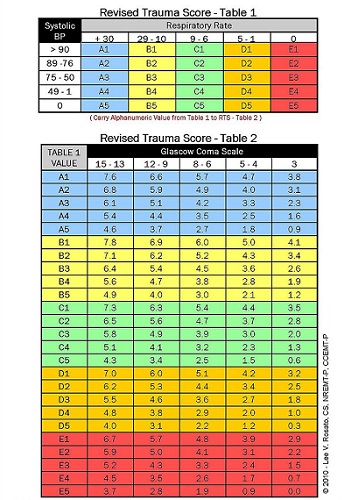
The initial version scored on fourteen different points; this was later increased to fifteen with the separation of extension and flexion within motor (movement) responses. In modern emergency, intensive care, and surgical settings the GCS is usually part of a wider group of scales such as the Acute Physiology and Chronic Health Evaluation (APACHE) II score, the Revised Trauma Score, the Trauma and Injury Severity Score (TRISS), and the Circulation, Respiration, Abdomen, Motor, Speech (CRAMS) scale.
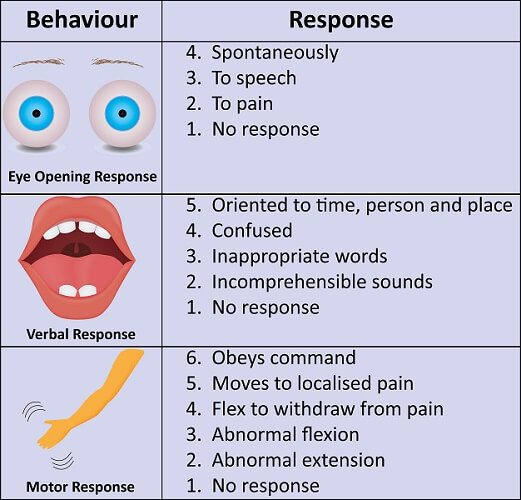
A GCS score is the result of eye movement, verbal reaction, and body movement assessments. These elements will be looked at in more detail in the next section.
Glasgow Coma Scale Score
The Glasgow Coma Scale score indicates levels of arousal and awareness; one does not naturally mean that the other is present.
Eye movement is an indication of arousal – by speaking to an individual who has their eyes closed, the eyes will usually open. Even so, a brain vegetative state does not mean that someone always has their eyes closed. People in a coma state can open their eyes to auditory stimuli.

Awareness is the ability of a person to interact with their environment and with themselves. Lower verbal forms such as moaning can be made when in a vegetative state.
A Glasgow Coma Scale of 8 or less indicates a severe injury that has dramatically affected the person’s state of consciousness. Scores between 9 and 12 indicate a moderate injury but are also normal scores in a recovery ward. Minor injuries rarely score less than 13 on a Glasgow Coma Scale assessment.
Three assessments are made, and it is important to note that the best responses should be measured, not the worst. If, for example, a motor vehicle crash victim switches rapidly between incomprehensible and confused speech, scores should be given for confused speech.
Eye Opening Response
As already mentioned, coma patients can open their eyes; this can affect the eye-opening response score given by the Glasgow Coma Scale. One study also reports that coma patients may close their eyes in response to pain rather than open them. However, as the GCS is now integrated into larger neurological function scores like APACHE II, its value as a medical scoring system is not affected.

Eye-opening responses score from a maximum of four to a minimum of one and are:
- Eyes open spontaneously
- Eyes open to verbal stimuli
- Eye open to pain
- No response
Verbal Response
Verbal responses may be the result of existing problems such as speech impediments, dementia, or an unrecognized foreign language; GCS results can change dramatically as a caregiver learns more about the patient.

A verbal response usually requires a conversation. This is why you will hear paramedics on TV shows asking a patient if they know what day it is or what their name is. Scores of 5 and 4 mean that a form of conversation between two people is occurring. Inappropriate words and incomprehensible speech do not allow for proper conversation.
- Oriented speech
- Confused conversation
- Inappropriate words
- Incomprehensible speech
- No response
Motor Response
Getting the top score of motor response may be affected by something as simple as a language barrier – a common problem for medical staff at international airports and tourist attractions. Asking someone who does not understand English to “stick out your tongue” will rarely get the required response.
To determine flexor or extensor posturing, medical staff usually use pressure on the nail bed as a pain stimulus.

- Obeys commands for movement
- Purposely moves in response to a painful stimulus
- Withdraws to pain
- Decorticate posturing (flexion) in response to pain
- Decerebrate posturing (extension) in response to pain
- No response
Decorticate posturing (above) relates to a stiff posture with bent arms, clenched fists, and straight legs. The arms are bent towards the body.
Decerebrate posturing (below) relates to a similarly stiff posture but with both arms and legs stretched, pointed (down) toes, and arched head and neck.
Glasgow Coma Scale Interpretation
Glasgow Coma Scale interpretation is not as simple as it might seem. Even medically-trained personnel have problems judging whether a patient is conscious or unconscious. Modern medicine also means that many trauma victims are intubated on-scene; it is impossible to measure awareness and arousal at this point. Even the administration of pain medication will affect results.
Patients who have been intubated on-scene will have an artificial Glasgow Coma Scale result and are usually assessed using the Full Outline of UnResponsiveness (FOUR) score.

Many variables make it difficult to observe the correct level of response. Facial trauma may make assessing eye movement difficult. A foreign victim might not speak the language of the emergency team and be unable to follow commands. A victim may be deaf. Alcohol and drug use can affect all three response parameters. Spinal cord damage will make motor responses and movements in reaction to pain unreliable.

The Glasgow Coma Scale range of scores is not just the sum of all three tests; it measures arousal, verbally-assessed awareness, and motor-assessed awareness separately. The total Glasgow Coma Scale score is a rapid way to determine victim response in an emergency but the separate parts are more important during longer-term care.
This means that score expression should be noted both as a total and per element, for example, GCS11 = E5V2M4.
A Glasgow Coma Scale 7 result would similarly be split into its elements. This is important for medical staff as GCS7 = E1V3M4 and GCS7 = E2V1M4 could indicate different treatments or diagnoses.

It is impossible to score 0; Glasgow Coma Scale 3 is the lowest possible outcome. Glasgow Coma Scale 15 is the highest possible score.
Pediatric Glasgow Coma Scale (PGCS)
Two pediatric Glasgow Coma Scales have been developed for children under five years of age. The first – for children under two years of age – is a non-verbal scale. The second uses verbal stimuli. Studies show that the PGCS is reliable for young children, especially in the pre-verbal stage.

The same three responses are measured – eye, verbal, and motor. These responses are also scored in the same way – eye response scores of 1-4, verbal response scores of 1-5, and motor response scores of 1-6.
Best eye response scores do not change in either of the pediatric Glasgow Coma Scale versions.
Changes are made to adapt to the pre-verbal responses of babies:
- Coos and babbles
- Irritable or crying
- Cries in response to pain
- Moans in response to pain
- No response
In the over-twos, these scores are:
- Oriented/appropriate speech
- Confused speech
- Incomprehensible words
- Incomprehensible sounds
- No response
The motor assessment of the pediatric Glasgow Coma Scale scores has also been adapted to fit the responses of the under-fives.
For babies and young toddlers (pre-speech):
- Moves spontaneously and purposefully
- Withdraws to touch
- Withdraws to pain
- Abnormal flexion to pain
- Abnormal extension to pain
- No response

For the under-fives (with speech):
- Obeys commands
- Localizes to pain
- Withdraws to pain
- Abnormal flexion to pain
- Abnormal extension to pain
- No response