Definition
Circadian rhythm describes the physical, psychological, and behavioral patterns of living organisms that respond to day and night light levels. Circadian rhythm is a subcategory of chronobiology that looks at how certain aspects of humans and other organisms respond to light and dark triggers. Internal biological clocks that extend from a master clock in the hypothalamus can become dysregulated, leading to health problems.

Circadian Rhythm Disorder
The Basics
Circadian rhythm disorder is listed as a sleep-wake schedule disorder in the International Classification of Diseases (ICD) that describes countless human physical and psychological illnesses. The ICD diagnostic tool also links circadian rhythm disorder to diseases of the nervous system and more generalized sleep disorders. To be diagnosed with a circadian rhythm sleep disorder a person might suffer from regular sleep disruption that leads to daytime sleepiness, or be unable to fall asleep and/or stay asleep. To suffer from circadian rhythm disorder there must be disorder in day and night patterns, for example, someone might find it hard to get to sleep because they work shifts or regularly take long-haul flights across different time zones. Another cause is damage to the nervous system that can affect the body’s multiple internal clocks. Circadian rhythm is just one of the many chronological patterns of the body; biological clocks regulate the timing of these patterns and decide when a female is fertile, or when certain hormones are released, for example.

Disturbed sleep-wake cycles are often seen in patients with Alzheimer’s disease. Other negative influences that upset the natural clock such as alcohol and recreational or prescription drugs can also cause wake-time sleepiness and the inability to sleep.
A circadian rhythm disorder is specifically the result of desynchronization between our inner sleep-wake rhythms and the light and dark cycle of our environment.
Treatment
Temporary circadian rhythm disorder treatment for short-term disruptions like long-haul flights can be counteracted by slowly changing the sleep-wake cycle in the week to two weeks before travel. Once at your destination, simply allowing your body to experience morning sun and evening darkness can help your body to adjust.
Shift workers may work fixed night shifts as well as suffer from other environmental factors such as noise, light, and social responsibilities when sleeping during the day. Keeping the bedroom dark and quiet and perhaps using a high-lux lightbox in the night-time hours when awake are non-pharmaceutical, proven methods of restoring circadian rhythm.
Changing bad sleeping habits under the guidance of a psychotherapist or psychiatrist is referred to as behavioral therapy. The treatment of a lack of synchronicity between a biological clock and circadian rhythm includes sticking to fixed hours for sleeping and waking, avoiding daytime naps, enjoying regular exercise, avoiding caffeine and nicotine, keeping the television, computer, and mobile device screens off in the final hours before sleep, and spending the hour before sleep in a restful state.

Environmental changes can also help circadian rhythm and include blocking out light in the bedroom, using relaxing paint schemes in areas of rest and stimulating colors in working spaces, trying earplugs and eye masks when sleeping, and implementing bright-light therapy to advance or delay sleep under the guidance of a trained sleep specialist.
Complementary treatments for circadian rhythm disorders are available over the counter but can do more harm than good. Melatonin, for example, is a naturally-released hormone released from the pineal gland when it gets dark. Melatonin is often taken as a natural supplement without medical support and this can make a sleep disorder much worse. The herb valerian is used as a supplement or tea to shorten the time needed to fall asleep but does not lengthen the actual time spend asleep – you should always be aware of whether you have trouble falling asleep or staying asleep before considering supplements. There is a lot of misinformation about that confuses circadian rhythm timekeeping with the chemicals that circadian rhythm regulates. This has led to unnecessary and sometimes harmful intake of supplements.
Pharmacological drugs for circadian rhythm disorders include melatonin and orexin receptor agonists, benzodiazepines, hypnotics, and modafinil. Many of these drugs have intense side effects that include daytime drowsiness. Taking them can affect a person’s ability to use machinery or drive a car that means all types of sleep medication should only be taken under the guidance of a medical professional.
Circadian Rhythm Regulation
Circadian rhythm regulation is controlled by circadian clock genes that are responsible for how our bodies adjust their physical and mental functions in the presence or absence of light. New evidence tells us that irregular circadian clock genes do not only cause sleep disorders but metabolic disorders (diabetes), psychiatric disorders, and even cancer.
Circadian rhythm regulation in mammals begins in a part of the brain called the hypothalamus that sits at the top of the brainstem. More specifically, tissue inside the hypothalamus called the suprachiasmatic nucleus or SCN is responsible for how our bodies respond to light levels. This part of the anatomy is sometimes called the suprachiasmatic nucleus pacemaker which gives us a clue as to its central role. Neurons in this part of the brain receive input via the optic nerve. The information the optic nerve delivers concerning how light or dark it is tells the SCN how and when to communicate with other cells. But there’s a catch – the SCN also produces rhythms that have nothing to do with light levels. How do we know this? Well, people who have had both eyes removed also have sleep-wake cycles, although these are very different from the patterns seen in people who can see.

Neurons directly in contact with the SCN are found in the immune, digestive, endocrine, cardiovascular, renal, and reproductive systems. The fact that the SCN is connected to so many different tissues tells us more about why obesity, infertility, and heart problems are partially linked to disturbed sleep-wake cycles.
According to the level of light, the master circadian clock of the suprachiasmatic nucleus signals to various areas of the brain that contain their own, local circadian clocks. These local locks contain regulatory cells that enable sleep and wake states, how big our appetite is, autonomic pathways that free blood glucose and triglycerides in the blood, and even modulate our cognition and mood. Fresh signals from these local clocks are then sent on to associated tissues that contain cells that express circadian rhythm genes.
Circadian Rhythm Effects
Circadian rhythm effects are multiple and many are probably still undiscovered. Further links between obesity, diabetes, mental illness, and hormonal imbalance with circadian rhythm disruption are being studied and it is obvious that this tiny part of the central nervous system is more than just a light-sensor.
The main physiological reactions to light levels are widely known. For example, cortisol secretion is regulated by the SCN; secretion is at its lowest at night (around 40 nmol/l) and at its highest (ten times more) in the morning. The hormone melatonin is an important regulator of seasonal rhythm (winter through to summer) and is responsible for weather-regulated breeding times and coat growth in mammals. In humans, low melatonin is a possible cause of Seasonal Affective Disorder (SAD) but can also affect our levels of fertility. This means that taking melatonin supplements for sleep disorders can have undesired effects on other systems. You may not grow a shaggy winter coat, but depression and an increased risk of infertility are definitely possible.

The hormone vasopressin is secreted in much lower levels during the night, allowing our blood vessels to relax which causes a fall in blood pressure. The SCN messages secondary oscillators in the kidneys, brain, and cardiovascular system. Blood pressure has its lowest levels at night, experiences a morning surge, then has its highest peak in the mid to late afternoon. As blood pressure is the result of the amount of blood pumped through the heart (cardiac output) and how much pressure the blood exerts upon blood vessel walls (peripheral resistance), blood pressure measurements indicate the health and function of the entire cardiovascular system. It is interesting to note that long-term irregular shift work that spans night and day shifts is associated with an increased risk of cardiovascular disease due to chronic hypertension.
Circadian Rhythm Effects in the Brain
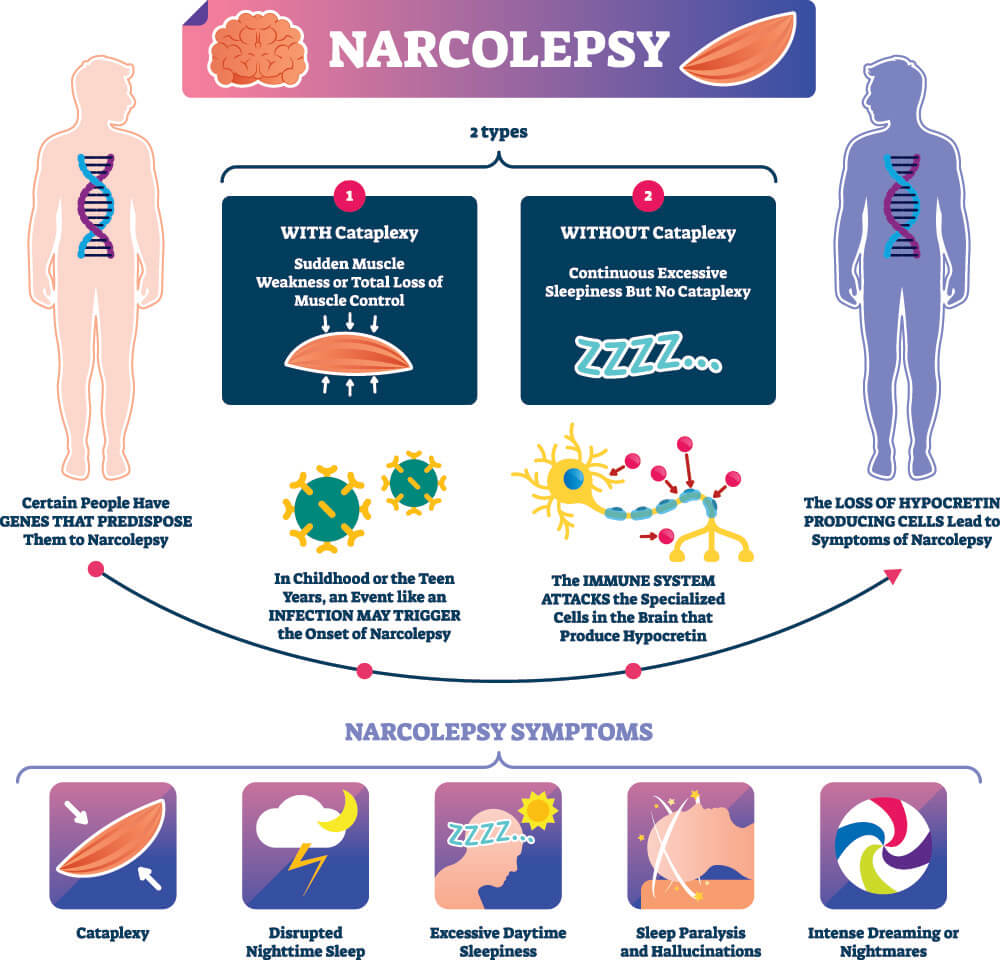
One neuropeptide (protein necessary for brain function) that is worth mentioning is orexin or hypocretin. Orexin neurons in healthy individuals fire non-stop during the day and are practically silent when they are asleep. In people diagnoses with type I narcolepsy (narcolepsy with cataplexy), these orexin-containing neurons are lost. The effects mean less dopamine, norepinephrine, serotonin, and histamine production in the brain – very important neurotransmitters when it comes to staying awake and alert. The symptoms of narcolepsy are severe daytime sleepiness with regular (daytime) lapses into deep REM sleep. Narcolepsy is on occasion paired with cataplexy – a temporary (seconds) phase of muscle weakness that is triggered by excitatory stimuli. As these excitatory stimuli are mediated by the above-mentioned neurotransmitters, the link between narcolepsy and cataplexy is easy to make. Furthermore, narcolepsy is associated with sleep paralysis, hypnotic hallucinations, and obesity. This shows the strong associations between the master clock of the SCN, the secondary oscillators of the brain tissue, and the presence or absence of circadian rhythm gene expression in various tissues. In short, circadian rhythm does not only provide a sleep-wake function but is essential for multiple primary functions.
Circadian Rhythm Effects on Other Systems
Not enough is known about the complete range of circadian rhythm effects on other systems. The items mentioned in this article scratch the surface and further roles and associations will most definitely be uncovered in the future. Important survival mechanisms such as body temperature control are also linked to the sleep-wake cycle. For example, when the body temperature rises or falls beyond normal ranges, people tend to become sleepy. This is an energy-conserving action.
However, tiny differences in temperature keep the various biological clocks synchronized. Whenever the SCN receives visual information from the optic nerve, it forwards some of this information as temperature-setting data. Temperature is, therefore, an important regulator of physiological and psychological health but not in the same way that our body temperature rises on a hot day or drops when outdoors in the winter without a coat. Instead, the SCN changes the body temperature by tiny increments; we don’t feel the changes but our internal physiological systems do. We have also learned that SCN neurons are not themselves temperature-sensitive. So we can say that SCN signals are not affected by the surrounding temperature of the environment or the tissues, but the SCN uses tiny temperature differences as a means of communication.
In the gastrointestinal tract, circadian rhythm tells cells when to secrete digestive enzymes and hormones. A good night’s sleep aids digestion – you will have heard this on all kinds of health advertising channels – and the marketing departments are right. It is when the body is sleeping that the secondary oscillators in the gut are activated. Of course, it’s not that simple; the gastrointestinal tract and liver also produce their own circadian rhythms that have nothing to do with light exposure and may not be synchronized with the master clock of the SCN. We can actually adjust these patterns by changing how and when we eat. For example, chronic alcohol use induces circadian time misalignment by altering the timing of the secondary liver clock. It is also suggested that desynchrony between gastrointestinal secondary oscillators and the central clock could be a major factor in the development of digestive disorders, insulin resistance, diabetes, psychological health, and even a weakened immune system.

From health to chronic disease, the internal master circadian clock plays a leading role. While research into this field of physiology and psychology is still in its early stages, improving health at every level might begin with making the simple but effective distinction between night and day activity and rest.
