Definition
A cancer cell is a natural but immature cell in the body that has developed mutations in its DNA. These mutations cause repetitive, unregulated cancer cell division that leads to similarly mutated, non-specialized daughter cells that themselves continuously divide. A cancer cell grows and multiplies – that is its sole, abnormal function. As this process continues through time, cancer cell proliferation causes solid tumors and/or blood cancers.
How Does a Normal Cell Become a Cancer Cell?
A cancer cell develops from a normal cell by way of one or more mutations in the DNA. Our DNA is packaged into chromosomes – tightly wound and copied strands of code that are only partially protected from the environment. While one mutation may not cause any effect, the older we become, the more irregular mutations we inherit from our parents, or the unhealthier our lifestyle, the more these different mutations accumulate.
Each coding gene gives instructions that produce a particular protein within ‘switched on’ cells. Our bodies rely on proteins – they make up all of our tissues and also the chemical messengers that make the body function, including neurotransmitters, hormones, and chemokines. Proteins form the receptors on the outside of cell membranes that accept chemical messengers. Not every cell has the same receptors, although every cell (except the anucleate red blood cell) contains the instructions to make them. A coding gene must be switched on or ‘expressed’ in a cell for a particular protein to be produced.
Other areas of the DNA that do not code for protein synthesis – called noncoding DNA – switch gene expression on or off according to cell type, organism age, and even according to the season or time of day.

Our DNA code is written using four specific proteins – adenine, thymine, guanine, and cytosine. Outside the nucleus, these lettered sequences can be read and their instructions followed. If the DNA is damaged and then repaired, any one of these four specific proteins can be reshuffled. Usually, this does not make much of a difference to cell function.
However, one tiny variant to the DNA of a cell is carried over to subsequent generations of daughter cells. If one or more of these cells also experience DNA damage with faulty repair, larger portions of damage can change the DNA code. Perhaps different proteins are manufactured, or no proteins, or too many, or too few. Perhaps the wrong cells start to produce the wrong or faulty proteins.
When cell growth is affected – in which we include changes in cell division, maturation, division, and death – cancer cells are the result.
A normal cell becomes a cancer cell when the DNA is damaged in such a way that the cell growth cycle changes. A cancer cell is a non-functioning cell that does not die when it should but continues to divide, passing on its malfunctioning DNA to daughter cells that are also cancer cells. Growth for the sake of growth is the ideology of the cancer cell.
The causative factor that turns a normal cell into a cancer cell is the cause of the DNA mutation. There is rarely a single cause. Causes might include a lack of antioxidants in the diet, working without protection in an asbestos factory, chronic inflammation, sunbathing without sunscreen, and inherited mutations.
Gene Variant Causes
There are two main groups of gene variants (mutations). These are inherited and non-inherited. Some are good for us. Without mutations, there would be no diversity of species. However, DNA damage can have less positive influences, too.

Inherited gene mutations are passed on through generations – a baby born to two parents with type one diabetes has a near one-in-two chance of having this genetic form of diabetes. Some inherited gene mutations are de novo. The mutation occurs in the sperm of the father or the egg of the mother and the gene variant occurs during fertilization, passing on this DNA to every cell of the growing embryo. If the gene variant exists in proteins that only form later on in life, such as certain hormones during puberty, symptoms may be absent until a later date.
Currently, very little can be done to prevent inherited gene variants. The use of genetic engineering to alter genes at the earliest stages of embryo development produces an intricate web of ethical issues that, as yet, keeps this area of study strictly in the laboratory. Inherited cancer is rare; however, inherited cancer syndromes increase the risk for developing certain cancers. One example is ovarian cancer that often develops in females born in families carrying the gene for hereditary breast and ovarian cancer syndrome. Another example is the increased risk of colon cancer in people from families that carry the hereditary non-polyposis colorectal cancer gene.

Non-inherited gene mutations happen during our lifecycle and only affect individual cells – these can be spread throughout the body or be of the same tissue type. A mutation or gene variant does not always cause cancer but it can cause illness, over time. As subsequent generations of cells divide to produce the variant of the original cell, a problem might become evident.
The causes of non-inherited gene mutations are many. Inhalation of asbestos dust can damage the DNA of lung cells, as can tobacco smoke, radon gas, and soot. All are carcinogenic – they have the potential to create cancer cells.
Obesity increases the risk of developing colorectal, esophageal, kidney, and pancreatic cancer, probably due to a chronic inflammatory state. Infections can also damage DNA and lead to cancer cell development. Remember that only mutated cells that grow uncontrollably are cancer cells.

Ultra-violet radiation and x-rays are sources of non-ionizing radiation that break DNA bonds. When the DNA is repaired incorrectly or radiation exposure continues, there is a higher chance of a cancer cell developing. The larger the area of exposure, the higher the number of potential cancer cells produced. Radiation in the form of computer tomography scans or as cancer treatment is much less likely to cause gene variants than stronger, non-ionizing forms.
Alcohol is another carcinogen that, over time, affects the DNA of cells in the digestive tract, airways, and liver. This is mainly the effect of the carcinogen acetaldehyde that is produced during the breakdown of alcohol.
For those that think drinking tea is the safest alternative, frequently drinking very hot beverages burn esophageal cells and damage their DNA. During nitrogenous base repair, faulty mutations inside the scalded DNA can occur.

The current list of known mutagens is much too long to list within this article. Length of exposure, age of exposure, other risk factors, and cell division time means that no mutagen is predictable. Not all smokers or morbidly obese people develop cancer, although greater proportions of these groups do in comparison with non-smoking or low body mass index groups.
Cancer Cell Cycle
The cancer cell cycle uses the same mechanisms as a normal cell, but this process is highly unregulated. The normal mammalian cell cycle has five phases.
Between the stages of cell division lie interphases that last at least 12 hours. These ‘resting’ stages or gap phases are badly named; most are periods of intense protein synthesis. Proteins are essential as they make the dividing cell grow big enough to divide. The interphase occurs four times per cycle – Gaps 0, 1, and 2, and the Synthesis (S) phase.
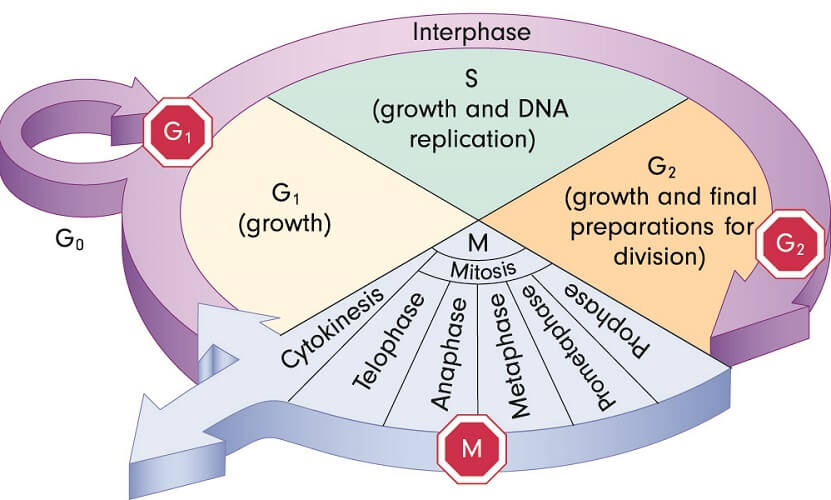
During Gap 0 (G0), the cell is considered out of the cycle. This is the only ‘resting’ interphase. How long a cell remains in this resting period is guided by our non-coding DNA. Non-replicating cells do not divide for a temporary period (quiescent cells) or permanently (senescent cells).
During Gap 1 (G1), cells grow larger and produce more proteins. A G1/S checkpoint ensures that the cell is ready to move into the next phase – Synthesis.
At the Synthesis phase (S), the cell must replicate its DNA as it will divide to produce two daughter cells. Each daughter cell must contain a full set of chromosomes to survive.
Gap 2 (G2) signals the end of DNA replication and another period in which more proteins are produced; the cell has another chance to grow in size. Yet another checkpoint ensures the cell is ready to divide. This occurs in the M phase.
At the mitosis (M) phase, the cell stops growing and uses its energy to divide into two identical daughter cells. The M phase involves several steps – prophase, prometaphase, metaphase, anaphase, telophase, and cytokinesis. Mitosis only lasts for an hour or two in mammals and includes a metaphase checkpoint that ensures everything is running smoothly.
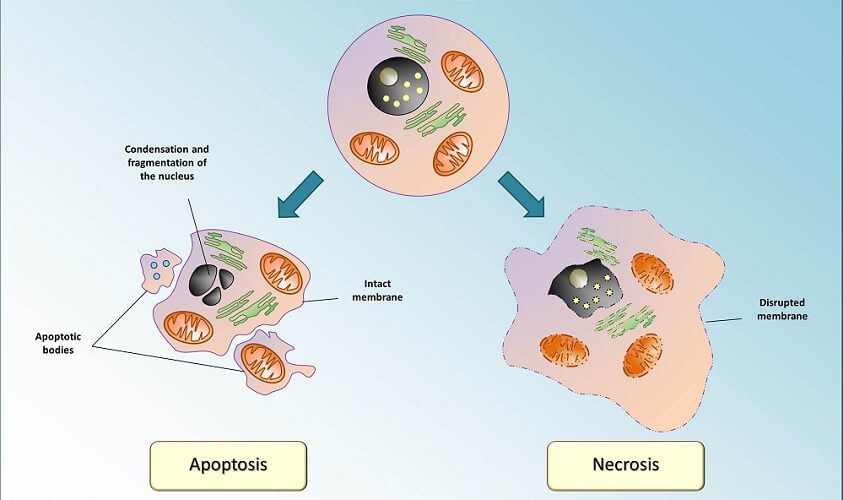
When errors are found at the checkpoints, a normal cell will usually enter apoptosis and self-destruct.
Cancer cell division, however, does not follow the rules of the regulatory checkpoints. With the majority of cancers, gene variants occur in the genes that code for regulatory proteins of the cell cycle. It has been found that the p53 protein malfunctions in more than 60% of cancers. Other regulatory chemicals such as cyclin-dependent kinases bind to proteins called cyclins and, upon doing so, start or stop the cycle.
A cancer cell cycle image would show checkpoint, growth, division, and cell death (apoptosis) anomalies.
Any gene that interferes with regulatory protein synthesis can lead to continuous cell division and the inability of a damaged cell to self-destruct. As all daughter cells receive the same DNA, a snowball effect occurs.
Cancer cells do not grow more quickly than normal cells, but they do not self-destruct and have no limits to how often they divide. Other types of cancer cells divide and grow normally, but live for much longer than their usual lifespan.
Cancer Cell Vs Normal Cell
The difference between a normal cell and cancer cell is spread across a range of characteristics. Normal cells reproduce according to regulatory signals in the DNA. For example, while nearly all of our cells contain the DNA code that codes for the entire human body, only a select group of information is available to a particular group at a particular time.
A white blood cell contains the DNA code to produce insulin, but this code – the insulin-producing gene – is only switched on in the beta cells of the pancreas. We say that the beta-cell expresses the insulin-producing gene. A white blood cell does not express this gene.
Regulatory genes control protein production. While coding DNA produces every protein required to produce the cells, tissues, and organs of the body, non-coding DNA tells cells when and in what quantities to produce them. Gene expression also controls when a cell grows, matures, stops growing, and divides.
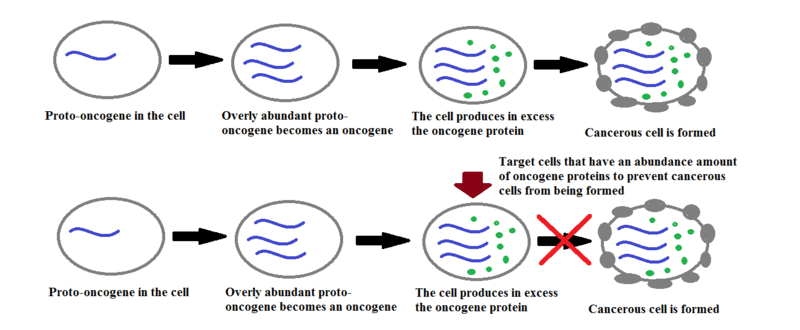
In cancer cells, mutations either stop certain proteins from being produced or they stop regulatory genes from working properly. Any gene involved in normal cell growth and division is called a proto-oncogene.
Cancer cells do not stop growing or dividing. Instead, one or more of their proto-oncogenes mutates into one or more ‘oncogenes’ – changes to DNA sequences that contribute to cancer development. This usually occurs when too many proto-oncogenes are produced within the cell. New cancer medications look at stopping cancer cell development by targeting these cells, as seen in the image below.
Another system that regulates cell growth and death is a group of proteins called growth factors. Cells have receptors for a wide variety of growth factors that tell them when to divide, mature, and die. When the DNA of a cell mutates to become a cancer cell, any of the estimated 30,000 genes in the human genome can be affected. A cell may develop more or fewer receptors for growth factors, be unable to understand the signals, or understand the instructions incorrectly. This leads to irregular cell growth.
Cells in which the DNA is damaged beyond repair are ordered to self-destruct (apoptosis). Normal cells rely on specific proteins that carry out continuous checks on DNA health. These are called tumor-suppressor genes as, by destroying badly-damaged cells, no mutated daughter cells carry on the cancer cell cycle; the original cell is dead and cannot reproduce. Without tumor suppressor proteins, cancer cell tumors can form.
Other genes that are commonly remodeled (mutated) due to pollutants, radiation, unhealthy lifestyles, and any of the countless risk factors for cancer cell development are those that produce cell-adhesion molecules or CAMs. Large groups of normal cells stick together to produce tissues – bone, liver, skin, or muscle, for example. With mutations in CAM-producing genes, cancer cells no longer adhere to their tissue type. This is the basis of metastasis or the movement of cancer cells through the fluids of blood or lymph. These cells can then relocate to other tissues such as the lungs, brain, or liver as metastatic cancer cells.
Another difference between cancer cells and normal cells is cell specialization. When a cell becomes specialized it can carry out its allotted function. A beta cell produces insulin, a muscle cell contracts and relaxes, a white blood cell protects the body from bacteria and viruses. With cancer cells, there is no specialization as these cells never mature. All cancer cells are non-functional.
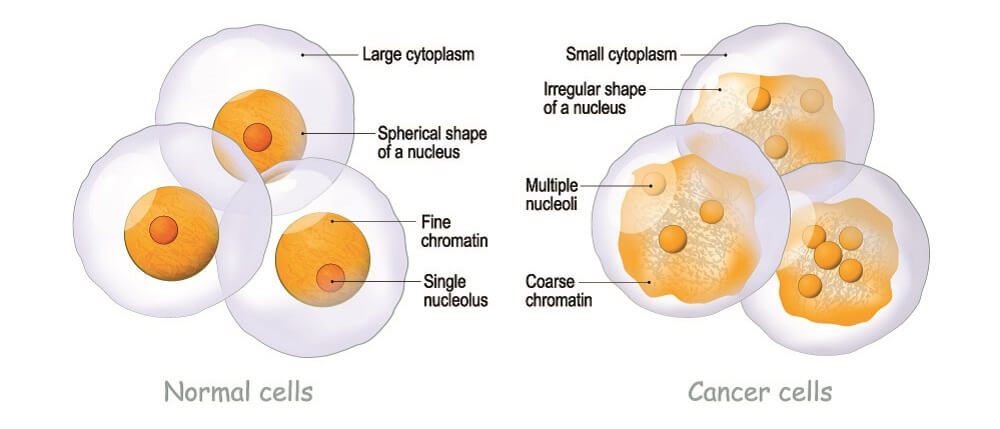
Physical differences between a normal cell and a cancer cell also exist. Cancer cells tend not to be all the same shape and differ from the cell they were intended to be. This can even be seen in the nucleus; a cancer cell nucleus has membrane blebs (bulges). Scientists are still looking at why cancer cell nuclei look abnormal.
Research into this dreaded disease is moving forward; however, cancer is still one of the world’s top killers with lung and colon cancers top of the list. Scientists study cancer cell lines by propagating one cancer cell over time and under laboratory conditions. These lines can be studied to understand how cancer develops and to test a rapidly growing range of updated and new cancer treatments.