Definition
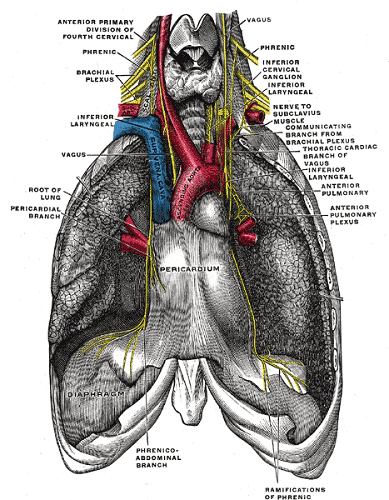
The paired phrenic nerve controls movement and provides sensation in the diaphragm, an important respiratory muscle. It is a mixed nerve that originates at the cervical vertebrae and ends where it merges with the solar plexus of the abdomen. The left phrenic nerve innervates the left side of the diaphragm and the right phrenic nerve the right. Motor nerves provide contraction during inspiration; sensory nerves transmit pain and movement sensation in the central diaphragm and the membranes surrounding the lungs (parietal pleura) and heart (pericardium).
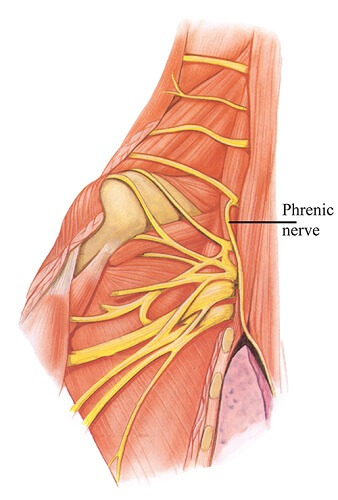
Phrenic Nerve Anatomy
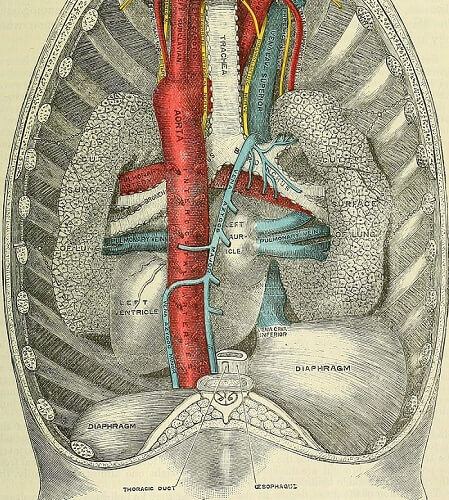
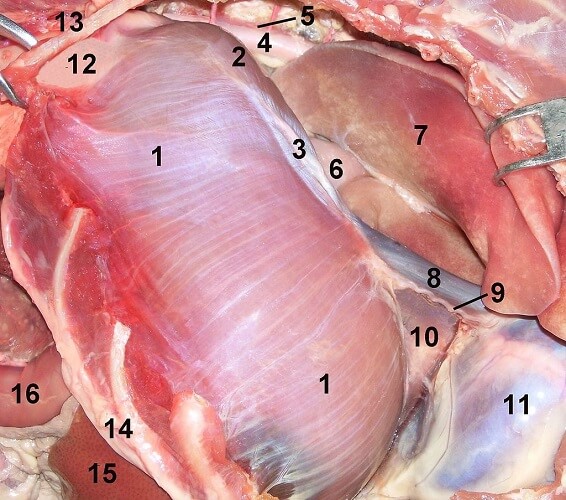
Phrenic nerve anatomy describes a peripheral (not central) nerve that is fed oxygen and nutrients via the pericardiophrenic artery (a branch of the internal thoracic artery); the parallel superior phrenic veins flow into the azygos vein (the central, pale blue vessel in the image below).
The diameter of the phrenic nerve is approximately 1.1 to 1.2 mm. Around 30% of the total surface area is composed of myelinated axons. Where non-myelinated fibers are found, many tyrosine-hydroxylase-positive (TH positive) fibers are present. These are particularly concentrated in the neck and right thoracic region.
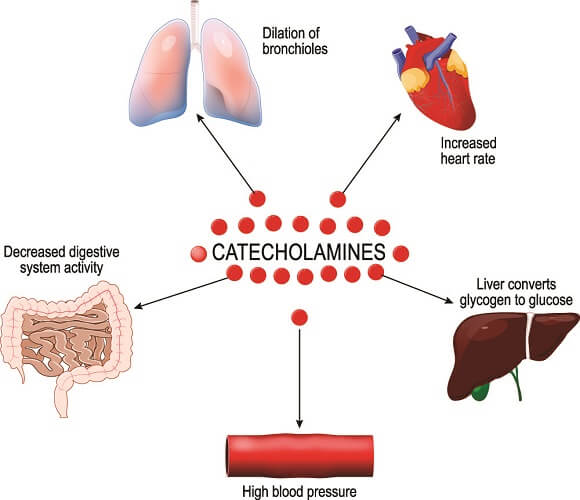
TH-positivity is a biological marker that indicates catecholaminergic nerve impulses. Catecholamines are the neurotransmitters dopamine, norepinephrine, and epinephrine. These transmit messages within the autonomic nervous system and are part of the complex autonomic cardiorespiratory system.
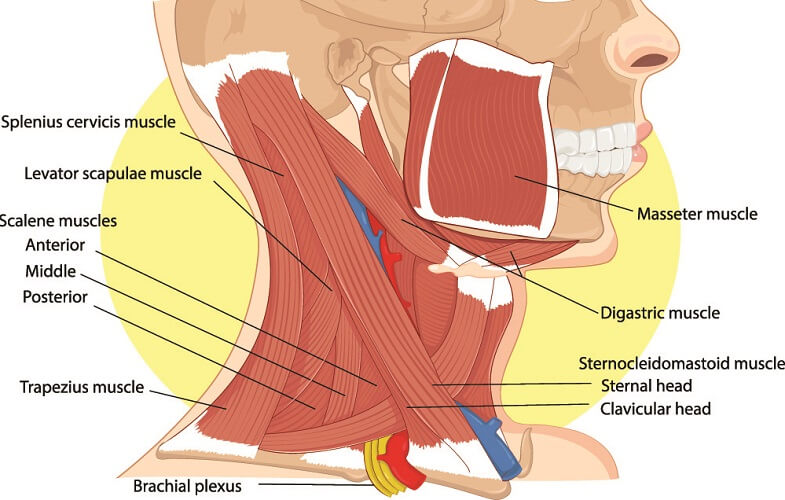
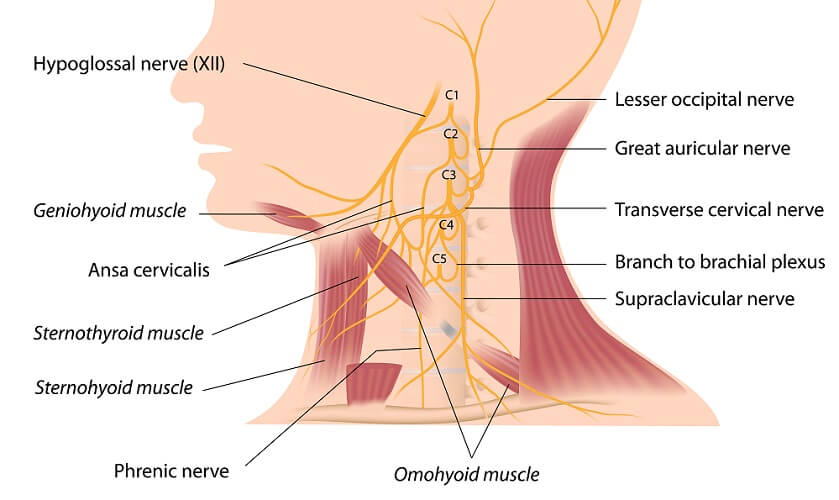
Phrenic nerve origin is at the nerve roots of cervical vertebrae three, four, and five; more specifically at the anterior rami. Phrenic nerve insertion points run throughout the thoracic space. The nerve ends where it merges with the celiac (solar) plexus.
The left and right nerves are composed of motor, sensory, and sympathetic fibers. The motor fibers control muscle (diaphragm) movement; sensory nerve cells control touch and pain sensations; sympathetic neurons are responsible for our breathing patterns. Increased sympathetic activity is linked to higher rates of morbidity and mortality in people suffering from central sleep apnoea.
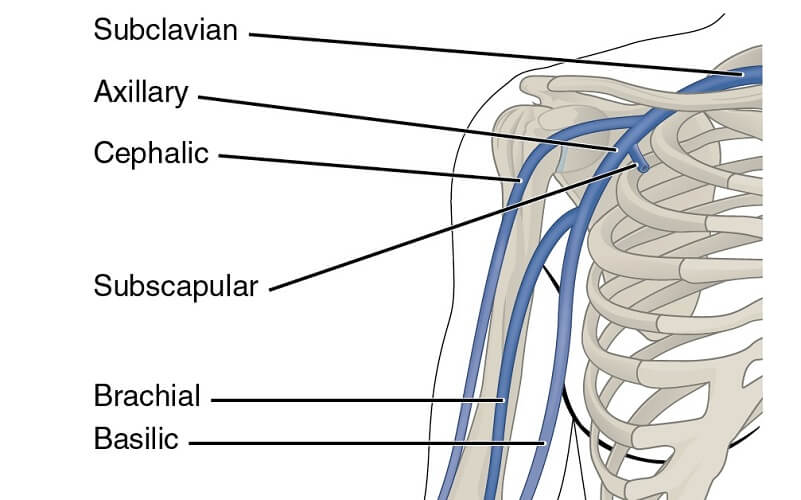
The phrenic nerves contain nerve fibers from other important nerves. These are the subclavian and sternohyoid nerves, the ansa cervicalis, and the aortic autonomic plexus. How much these nerves communicate differs from person to person.
The phrenic nerve pathway follows the course of the subclavian vein (see above). Phrenic nerve location begins at the lateral borders of the anterior scalene muscle (one of three scalene muscles indicated in the image below). It descends under this muscle before splitting. Left and right branches then change course; the right nerve is shorter and descends almost vertically. The left nerve is longer as it must navigate around the heart; the diaphragm is also slightly lower on the left side of the body.
Right Phrenic Nerve Location
The right nervus phrenicus runs over the right subclavian artery and enters the thorax. This occurs at a point called the superior thoracic aperture. The nerve then travels down the inside of the chest close to the right lung hilum. The right phrenic nerve innervates the pericardium of the right atrium and the right pleura as it travels between these membranes. It descends to where the inferior vena cava leaves the thoracic cavity via an opening in the diaphragm. It is here that the underside (inferior surface) of the right side of the diaphragm receives motor, sensory and sympathetic control.
The image below shows the phrenic nerve (9) to the side of the right lung (7). It lies close to the esophagus (6) and the sac covering the heart (11). The curve of the ribs can be seen at number fourteen and the final rib at number thirteen.
Left Phrenic Nerve Location
The longer left nerve leaves its opposite partner close to the mid-section of the left subclavian artery. It also enters the thorax via the superior thoracic aperture. Running close to the left lung hilum, the left nerve runs across the arch of the aorta. It then moves downward to innervate the pericardium at the left ventricle before reaching the underside of the left diaphragm.
Phrenic Nerve Function
Phrenic nerve function is integral to the cardiorespiratory system. As its fibers enter the pericardium, pleura, solar plexus, supporting ligaments of the liver, peritoneum, and even the adrenal glands that sit on top of the kidneys, phrenic function is also broad.
Motor Function
The left and right efferent motor fibers innervate the left and right hemidiaphragm (diaphragm halves) respectively. These are the diaphragm’s primary innervation pathways. Motor signals arrive at the muscle from the central nervous system and sensory information is transmitted back.
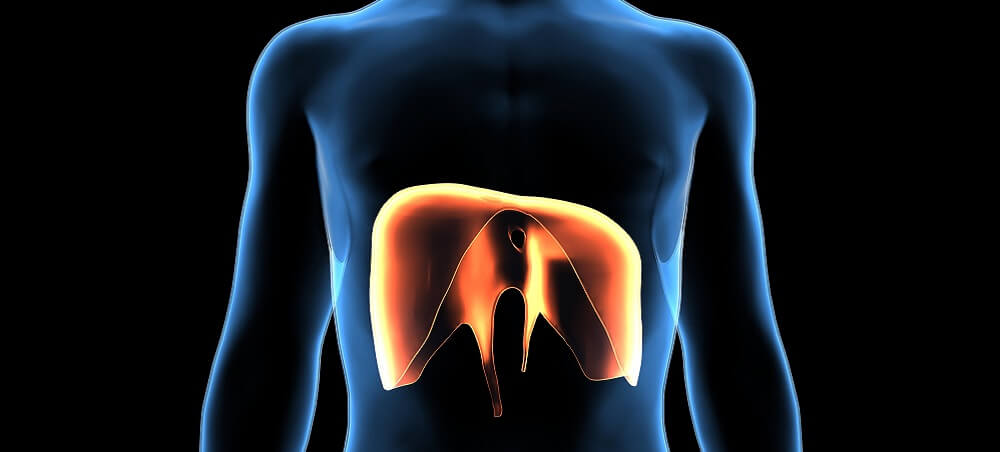
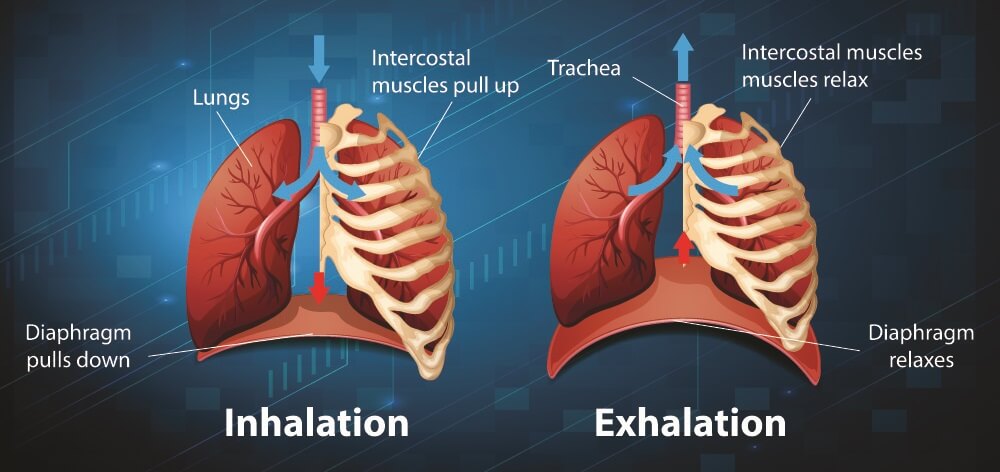
When we inhale, the diaphragm contracts. This creates a downward motion. Innervation of the external intercostal muscles that surround the ribs by the spinal nerves pulls the rib cage upward. Phrenic nerve stimulation is responsible for the contraction of the diaphragm.
When the diaphragm contracts and the rib cage lifts, the thoracic cavity expands. This pulls the lungs outward; air is pulled in.
Relaxation of the diaphragm occurs simultaneously with internal intercostal muscle contraction, although these are innervated by the spinal nerves. This decreases the volume of the thoracic cavity and the lungs are compressed, pushing air through the windpipe and out through the mouth or nose.
Phrenic nerve damage can cause breathing disorders. Phrenic nerve pacing, where electrical pulses stimulate the nerve and cause the diaphragm to contract, can postpone the need for mechanical ventilation.
Sensory Function
Sensory nerve fibers also innervate the diaphragm. Approximately 35 to 45% of the fibers are sensory; most of these are unmyelinated. As phrenic afferent nerves travel upward, diaphragm pain may be felt in the shoulders. This symptom is called the Kehr sign.
The nervus phrenicus supplies the brain with sensory information about the diaphragm, pericardium, and lungs, especially in regards to pain (somatosensation). There are a few proprioceptive fibers present which supply positional information. These may provide additional respiratory information for the autonomic nervous system.

Autonomic control (involuntary control of the diaphragm) triggers changes in breathing rate, depth of respiration, and arterial blood pressure. Our blood pressure changes slightly due to volume changes in the thoracic cavity when breathing. This nerve also responds to voluntary commands – we can opt to hold our breath or change our breathing patterns. But when carbon dioxide levels increase in the blood, the autonomic system takes over – we are forced to breathe in.
Other communicating nerves merge some of their fibers with the phrenic nerve. These are the subclavian nerve of the subclavian muscle, the ansa cervicalis that innervates the geniohyoid muscle of the tongue bone, and the thoracic aortic plexus that provides sensory innervation of the chest. While the phrenic nerve does not contribute to these structures as a primary nerve, communication between fibers means that all work together in some small way.
Phrenic Nerve Damage
Phrenic nerve injury often results in respiratory symptoms that can be mild to severe. Total paralysis of the diaphragm usually means suffocation without implementation of mechanical ventilation. This involves placing an endotracheal tube through the throat, between the vocal chords. The tube ends just above where the left and right bronchi bring air to the left and right lung respectively. A machine provides the correct mix of respiratory gases and breathing rates and breathing volumes can be adjusted.

Phrenic Nerve Irritation
One mild but potentially chronic pathology is phrenic nerve irritation – the hiccups. These reflexes are sometimes due to phrenic damage. Hiccups are spasms of the diaphragm. Hiccups may, less commonly, be caused by heart failure, stroke, meningitis, trauma, cancer, cysts in the neck that press on the phrenic nerve and vagus nerves, inflammation of the digestive system, and metabolic illnesses that affect nerve function.
One of the symptoms of pericarditis is hiccups. As we know that sensory innervation in this region is provided by the phrenic nerve, this is not surprising.
Persistent hiccup (singultus) continues for more than 48 hours. Hiccups that last for weeks or months often have no known cause. In serious cases, a procedure called phrenic nerve clipping reduces the number of nerve impulses to the diaphragm. However, due to the importance of the respiratory system, this is rarely recommended and does not always work.

Phrenic Nerve Paralysis
Surgical phrenic nerve damage usually affects the right or left branch. When one side of the diaphragm can contribute to breathing, symptoms are less severe. Even so, shallow breathing can increase the risk of respiratory infections and reduce oxygen levels throughout the body.
When both phrenic nerves are injured – most commonly due to brain or neck damage – the necessary nerve impulses fail to reach the phrenic nerve. Bilateral partial or total paralysis of the diaphragm is possible. Irregular sensory impulses can produce a lack of sensation or pain in the thorax and when breathing. If both sides of the diaphragm fail to receive motor impulses, severe and potentially fatal breathing problems are the result.

Neurodegenerative diseases like motor neuron disease and multiple sclerosis are associated with phrenic nerve palsy (paralysis) of varying degrees. Symptoms begin with increased respiratory infections and evolve into shortness of breath and cyanosis. Oxygen supplementation and then mechanical ventilation are necessary for severe cases.
Phrenic nerve paresis can also be caused by anesthetic nerve plexus blocks – most commonly the brachial plexus blockade. The anaesthetic spreads further than it should or the phrenic pathway does not follow the usual anatomical course. Once the local anesthetic loses its effect, the diaphragm recovers.

Poliomyelitis
The polio virus is spread via infected feces, food, and water. It affects motor fibers in the brain and spine, causing inflammation of the myelin sheaths – myelitis. Bulbospinal polio in particular affects the phrenic nerve. Symptoms evolve rapidly.
Before the polio vaccine was developed in the 1950s, cases were rife. Today, polio outbreaks are limited to Pakistan and Afghanistan. Occasionally, vaccine-derived polio is reported. Before vaccines, poliomyelitis epidemics led to large numbers of respiratory paralysis cases. Treatment was the famous iron lung. This very informative article tells the story of an English man infected with poliovirus in the late 1940s.