Definition
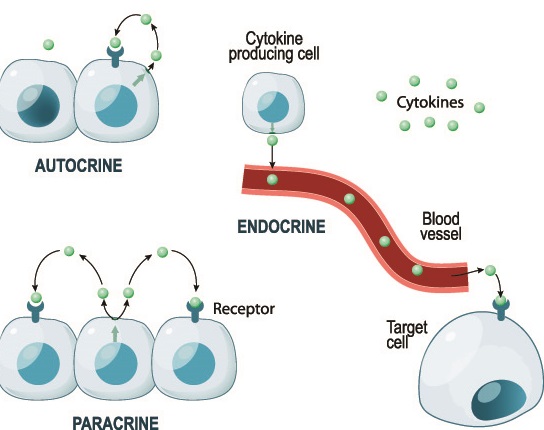
Dendritic cells are named after their shape and are not neurons with dendrites, as was thought when first discovered in the late nineteenth century. They are bone marrow and lymph-derived leukocytes or white blood cells. Dendritic cells play a primary role in immune responses. The ease with which they can be grown in laboratories together with their strong antigen-killing features makes them a promising anti-cancer agent.
Dendritic Cells Function
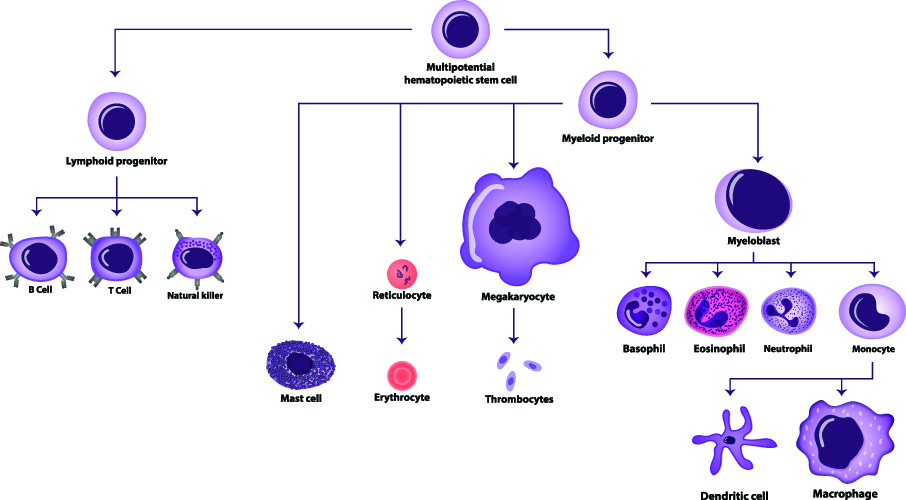
Dendritic cells function within the immune system. They are phagocytes and antigen-presenting or accessory cells (messengers and activators) in our innate and adaptive immune mechanisms. Dendritic cells are formed from precursor cells in the bone marrow and lymph tissue and are one of three types of antigen-presenting cells.
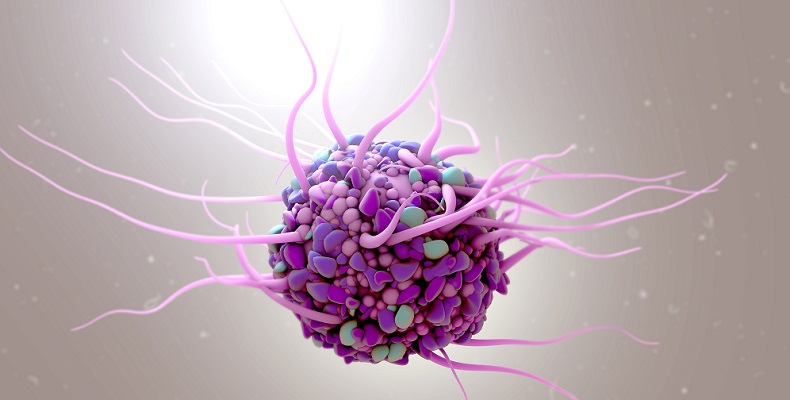
Antigen-presenting cells enable T lymphocytes to recognize and destroy antigens – foreign or toxic material. Without antigen-presenting cells, T lymphocytes would not react to potentially damaging particles that enter pr are produced inside the body. The three types of antigen-presenting cells (APCs) are dendritic cells, macrophages, and B-cells.
Found all over the body, dendritic cells concentrate in areas that contribute to immediate immune responses – lung, gut, blood, and lymphoid tissues. These tissues must withstand continuous antigen attacks.
Dendritic cells first appear as immature cells in these tissues and organs. Only after they have captured an antigen do they mature; only once they have caught an antigen are they called antigen-presenting cells (APCs). As APCs, mature dendritic cells migrate to the lymph nodes and present their captured antigens to T lymphocytes there.
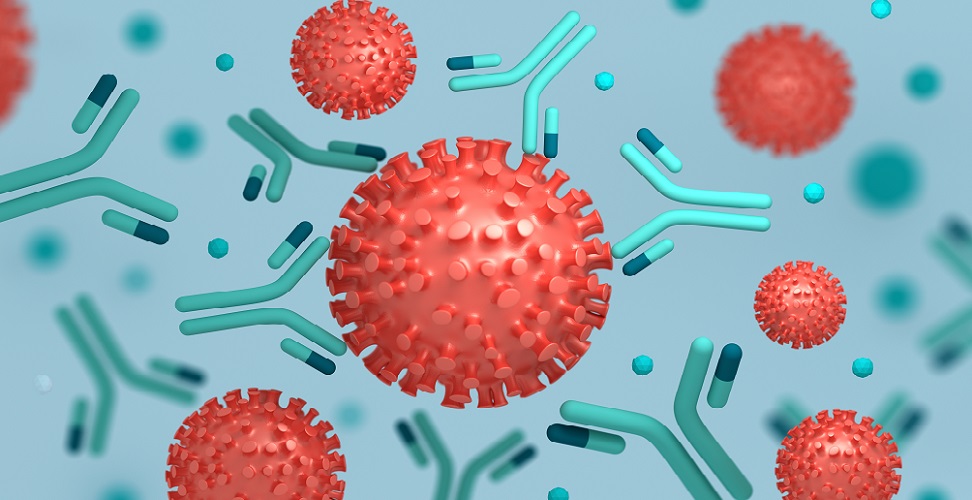
Dendritic cells have an important function in the innate immune system where they carry out surveillance duties, looking for antigens in the form of endogenous toxins and exogenous foreign substances. The presence of an antigen – or its surface proteins – stimulates an immune response. This is because certain patterns of molecules on the antigen or on damaged cell membranes make them recognizable. In the image, the orange antigens with many surface proteins have been detected by antibodies – the Y-shaped blue-green particles. Antibodies are a later stage of immunity that will be described further on.
Dendritic Cell Function: Innate Immune System
The innate immune system is a nonspecific mode of protection that occurs before, at, or within a short time of antigen exposure. Antigens range from viruses and bacteria to chemicals released from damaged cells when they are burned, scratched, starved of oxygen, or otherwise traumatized.
Most vertebrates have multiple protective barriers. These include skin, stomach acid, airway mucus, the blood-brain barrier, sweat, and tears. These anatomical barriers are part of the innate immune system.

If an antigen enters the body and survives despite these anatomical barriers, the next phase in the innate immune system defense mechanism takes over. All microbes have similar general patterns of molecules known as PAMPs (pathogen-associated molecular patterns) on their outer surfaces. Our pwn cells, when damaged, dying or dead, present with DAMPs (damage-associated molecular patterns).
The following image shows the invasion of pink antigen bacteria with PAMPs in the form of LPS (lipopolysaccharide) on their outer membranes. The macrophage has receptors for the LPS pattern that detect the PAMPS. Upon detection, the macrophage then secretes cytokines in response. Cytokines tell other cells that an attack is underway. The macrophage catches and digests the bacteria (phagocytosis).
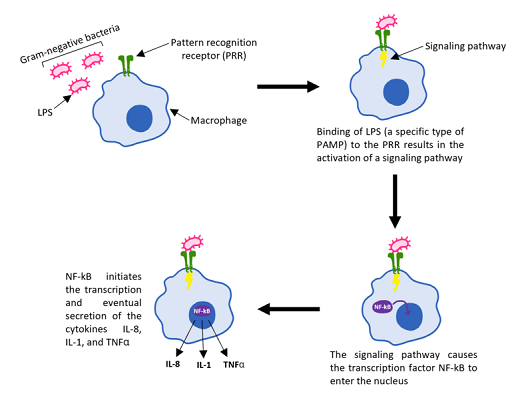
Many types of cells, including dendritic cells, have pattern recognition receptors (PRRs). A single pattern recognition receptor can recognize both pathogen- and damage-associated patterns.
The first step after PAMP or DAMP recognition is the inflammatory reaction. By increasing blood flow to the area, more white blood cells arrive to destroy the intruders. A fever helps, as many bacteria will die at temperatures higher than normal body temperature. Coughing and sneezing rids us of countless pathogens every day.
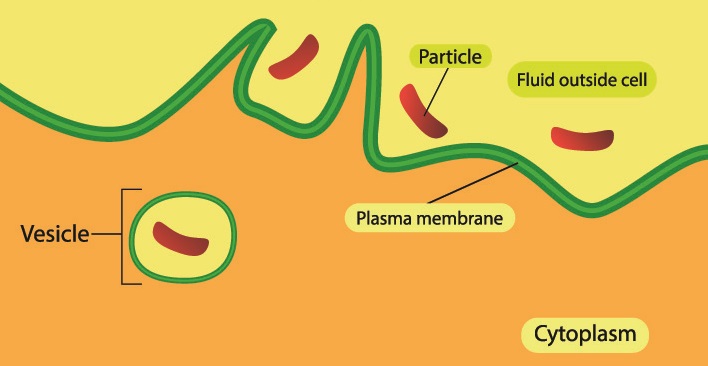
White blood cells release chemical factors such as histamine, prostaglandin, and bradykinin. These chemicals open local blood vessels and attract more phagocytic cells. Phagocytic cells wrap around foreign particles and toxins and digest them. Like macrophages and neutrophils, dendritic cells are phagocytes.
Macrophages and neutrophils scavenge and destroy harmful or foreign particles and release chemicals that attract more white blood cells. Dendritic cells perform phagocytosis and preserve information from ingested particles that can kick-start adaptive (acquired) immune responses.
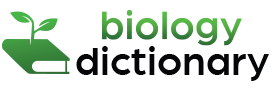
Cytokines are signaling molecules. This broad group includes interferons which you may recognize as the main component of some antiviral drugs. Cytokines stimulate or inhibit cell growth, cell death, inflammation, cell differentiation, and cell migration. They affect their own cell as autocrine messengers, neighboring cells as paracrine messengers, and travel through the bloodstream to affect more distant targets.
Dendritic Cells Function: Innate Immunity to Adaptive Immunity
Dendritic cells’ most important role after antigen capture is the activation of naïve T lymphocytes. Just like dendritic cells, a T-lymphocyte (T cell) changes its status when it comes into contact with and recognizes an antigen.
Naïve describes the original form of a mature T-lymphocyte as it leaves the lymphoid organ of the thymus. After a naïve T-lymphocyte has made contact with an antigen-presenting dendritic cell (or other APC type) it differentiates into an effector T cell. As an effector cell (causing an effect) it can destroy the presented antigen. An effector T cell is also called a cytotoxic T cell.
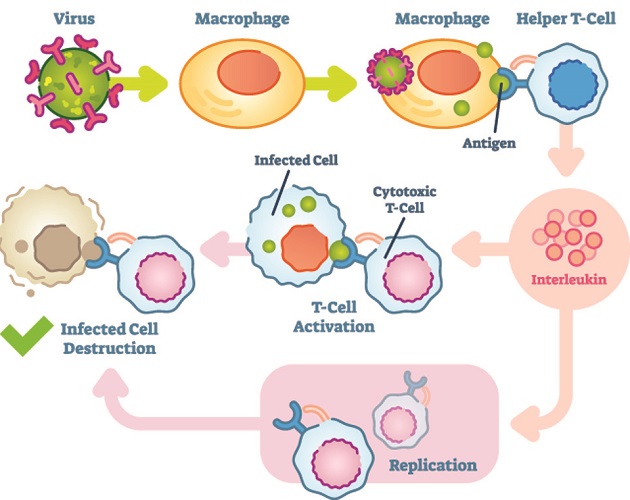
After an antigen has been destroyed, most effector T cells die; however, a small proportion differentiates into memory T-cells. Memory T-cells form the basis of our acquired (adaptive) immune response. They remember the antigen and are ready to attack if it enters the body again.
Dendritic Cell Types
In humans, dendritic cell types exist in three main groups. These are conventional dendritic cells, plasmacytoid dendritic cells, and epidermal (dermal) dendritic cells.
Plasmacytoid Dendritic Cells
Plasmacytoid dendritic cells originate in the lymphoid organs (lymph nodes, thymus, spleen, and tonsils) and the bone marrow. Lymph vessels and nodes (green) follow the same routes as our blood vessels (blue and red).
Plasmacytoid dendritic cells produce cytokines like type I interferon and tumoral necrosis factor. Cytokines stimulate the production of natural killer cells, B lymphocytes, and myeloid dendritic cells. They also have particularly strong antiviral properties.
Conventional Dendritic Cells
Conventional dendritic cells, also called classical or myeloid dendritic cells, are produced in the bone marrow and differentiate into three different types of cells once they reach the bloodstream. These types make their way to the lungs, intestines, liver, and kidneys.
Epidermal Dendritic Cells
Epidermal or dermal dendritic cells are found in different forms on and within the skin. All epidermal dendritic cells activate T-cells on or in the epidermis and dermis. One example is the Langerhans cell (LC). Langerhans cells migrate to the lymph nodes from the skin, bringing an antigen with them to present to a naïve T cell.

They do this by stimulating T cells to differentiate into T helper cells. This differentiation occurs in various glands close to the site of the antigen. T helper cells do as their name suggests – they help B cells to produce antibodies.
Other types of epidermal dendritic cells are produced in the bone marrow and differentiate in the blood and skin. Much of our knowledge of these cells is based upon rodent models – usually mice. We do not know exactly how these cells work in the human body.
The Immune Response
In humans, the immune response protects us from toxins produced inside the body and foreign particles and single-celled organisms that enter the body from outside. Antigens, as already mentioned, all have generic forms of surface proteins. Foreign microorganisms have PAMPs (pathogen-associated molecular patterns) and damaged cells or cancer cells have DAMPs (damage-associated molecular patterns). One molecular pattern receptor on an immune cell can recognize various PAMPs or DAMPs.

We possess many anatomical barriers against attack from the outside world. If we swallow a potentially harmful bacteria in our food, the acidic environment of the stomach is likely to kill it. If we breathe in a virus, it can get trapped in the thick mucus membranes of the nose before it reaches the more delicate region of the lungs. These are innate immune systems because we are born with them.
We are also born with phagocytic cells – macrophages, neutrophils, natural killer cells, monocytes, dendritic cells, etcetera. Phagocytes envelop and digest foreign particles, dead and damaged cells, and toxins. Dendritic cells are phagocytic and phagocytes are part of our innate immune system.
The other natural immune system is adaptive immunity. This system adapts or develops throughout life. It is here that dendritic cells play another important role, even though they are part of the innate immune system. It is often said that dendritic cells form a bridge between the innate and adaptive systems.
Whenever the innate immunity fails to stop a foreign particle from entering and multiplying inside the body, it is up to our adaptive immunity to remove it.
It takes time to develop our adaptive (or acquired or specific) immunity. All of our adaptive defense mechanisms are leukocytes or white blood cells. Leukocytes are split into two main categories – phagocytes and lymphocytes. While phagocytes form part of the innate immune system, lymphocytes rule the adaptive system.
Lymphocytes exist in two main forms: T and B cells. They are activated by antigen-presenting cells (like dendritic cells) that carry the foreign particles and pass them over so that the lymphocytes recognize them and destroy them or produce antibodies. The antigen-presenting cell carries an antigen to the lymphoid organs where immature T and B cells are stored.
T and B cells look very much the same but have different functions. T cells or T lymphocytes mature in the lymph nodes and thymus but remain naïve until activated. These cells do not have PAMP or DAMP receptors; instead, they are activated by antigen-presenting cells and cytokines.
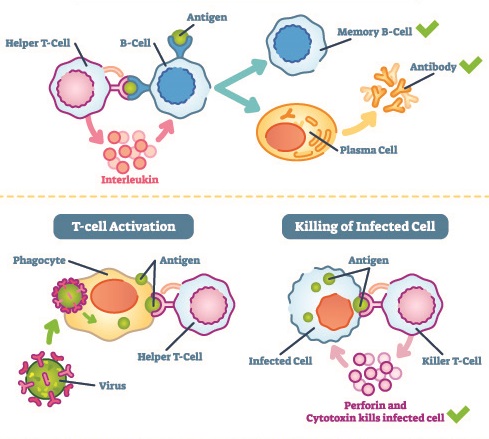
Once activated, T cells differentiate. Either they become short-lived effector cells or live for much longer as memory effector cells. As effector cells, T cells migrate to the area of inflammation. There they either function as a T helper cell or a T suppressor cell. T helper cells encourage other immune cells to release cytokines and kill foreign pathogens; they also stimulate B cells to secrete antibodies. T suppressor cells modulate immunity, preventing overactivity. Memory effector cells or memory T cells form from a small number of effector cells; they remember an antigen and respond quickly to a second attack.
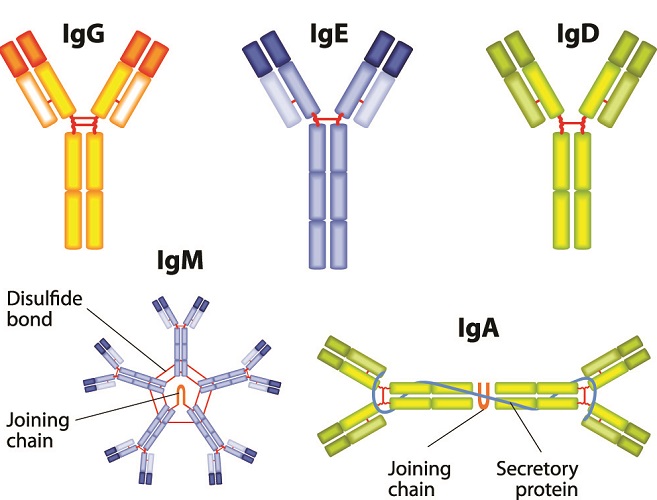
B cells or B lymphocytes produce antibodies or immunoglobulins. B cells have special receptors that bind to one type of antigen. These cells differentiate and mature inside the spleen but are naïve.
As with the T lymphocytes, B cells need to be activated. While T cells are activated by antigen-presenting cells and cytokines, B cells use their surface receptors to bind directly to an antigen. B cells can activate with or without the assistance of T cells; they are antigen-presenting cells.
Once activated, a single B cell multiplies into many clones. It is no longer naïve and is now called a plasma cell. Plasma cells secrete millions of antibodies into the blood and lymph. Every antibody recognizes and attacks the antigen that first came into contact with the naïve cell. These antibodies remain in the circulation for many months. Together with memory T cells they provide long-term protection against future infection.
Immunity and Vaccination
Vaccinations work either to provide an active acquired immune response or a passive response. When ready-made antibodies are injected into the body, they recognize a specific pathogen and attack it. This type of vaccination is relatively short-lived.
Other types of vaccines introduce a very small amount of pathogen – either alive but only mildly pathogenic (weak) or inactivated. It is then up to the dendritic cells and other antigen-presenting cells to start the process of building up an immune response and making sure T and B cells create memory cells and antibodies to prevent further damage. If you would like to know more about the different types of vaccines and how they work, the U.S. Department of Health and Human Services provides this overview.

Personalized dendritic cell vaccination is a new field of research that looks at using these cells as vaccines against cancer cells.
Dendritic Cells in Cancer Therapy
The use of dendritic cells in cancer therapy is under a lot of scrutiny. We need to understand how they work at a much deeper level to move towards personalized cancer treatment in the form of a vaccine or even a preventive pill.

Cancer vaccination is a form of immunotherapy. The ability of dendritic cells to regulate our immune responses is very relevant, as somewhere along the cancer route our immune systems fail to recognize abnormal cells and destroy them. As dendritic cells – and all antigen-presenting cells – can be fooled by cancer cells, loading them with a tumor antigen outside of the body before injecting them into the body could provide the right immune response. Cancer cells would no longer be left to proliferate without control.
Tumor cells suppress the activity of the immune system, including the activity of dendritic cells. This is because tumor cells hide behind their own anti-inflammatory cytokines. Not only are they very hard for an APC to recognize, they also block the natural inflammatory response of healthy immune cells. Cancer cells can grow unhindered and undiscovered.
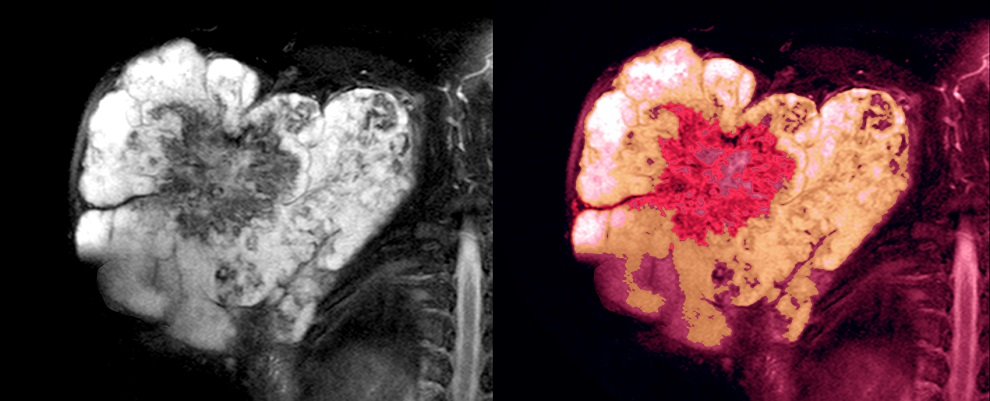
Dendritic cells are quite simple to grow in a laboratory. This makes them a popular choice for use in cancer vaccines. Current studies are looking at whether preloading dendritic cells with specific cancer antigens in the lab and injecting them into the body could be a future cancer cure. As the mechanism of immunity is not yet completely understood, and as personal physiological factors react very differently to treatment, trials produce fluctuating results.
Blastic Plasmacytoid Dendritic Cell Neoplasm
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare form of blood cancer. As its name suggests, the source of the cancer is the plasmacytoid form of dendritic cells. In BPDCN, cancer is caused specifically by plasmacytoid dendritic cells that produce high levels of type I interferon.
Blastic plasmacytoid dendritic cell neoplasm is more likely to affect middle-aged or older males. It presents as skin lesions and leads to acute leukemia.

Upon diagnosis, sufferers of BPDCN rarely survive for more than two years. The most visible symptom of BPDCN is red, lumpy skin lesions. Blastic plasmacytoid dendritic cell neoplasm treatment is chemotherapy. This treatment is initially very effective; however, in 90% of cases the cancer returns within a very short period.
Quiz