Definition
Seminal vesicles are secretory gland pairs found in the male gender of some mammals; these glands secrete specific components of seminal plasma. The seminal, prostate, and bulbourethral glands are the accessory glands of human males, but all three are not found in all mammals. Seminal vesicles are loosely-coiled structures surrounded by muscle. They are located in the pelvic region, more specifically under the bladder and behind the prostate gland.

Seminal Vesicle Function
Seminal vesicle function is limited to the male gender of some mammals. These two small glands have a secretory role – meaning they produce one or more chemical products and release them into the body. The seminal glands produce some of the components of semen. Without at least one functioning vesicular gland, a male of our species or any species that has them is unable to reproduce. So, what does the seminal vesicle do? To find out, it’s worth looking at the male reproductive system and its function in a little more detail.
Sperm cells are gametes (sex cells) produced in the testicles under the stimulation of the hypothalamus of the brain and the hormone testosterone. These cells contain the genetic information of the male that produces them and are composed of a head, body, and tail (axial filament). For a man to be able to reproduce naturally, millions of sperm must leave his body by way of ejaculation. How many sperm leave the body depends on many factors, but an average of 80 to 300 million sperm will leave the body at one time. Ejaculation is controlled by the sympathetic nervous system that triggers the muscular layers found throughout the reproductive tract to contract. This action pushes seminal plasma and sperm cells through the urethra. Seminal plasma and seminal fluid are not quite the same thing; the difference between seminal plasma and seminal fluid (semen) depends on whether spermatozoa are present – the mix of sperm and seminal plasma is called seminal fluid.
Without seminal plasma, sperm cells are unable to use their tails and move through the female reproductive system. Furthermore, as living cells, all spermatozoa require energy during their life-cycle. Seminal plasma – most of which is produced in the two seminal vesicles – allows sperm motility, protects sperm from the acidic environment of the vagina, stops them from wiggling around and moving too early (something that wastes a lot of energy), and provides a source of energy for the sperm cells.
Seminal plasma is composed of water, salts, carbohydrates, lipids, proteins, microbes, vitamins, hormones, and minerals. Curiously enough, seminal glands are not found in every male mammal – carnivores do not have seminal vesicles but produce their seminal plasma in the prostate gland. It has been suggested that humans are, evolutionarily speaking, herbivores, but this is only a very loose theory – rabbits do not have them and, so far, we don’t have carnivorous rabbits. No-one is sure why some mammals have seminal glands and others do not.

Seminal Vesicle Anatomy
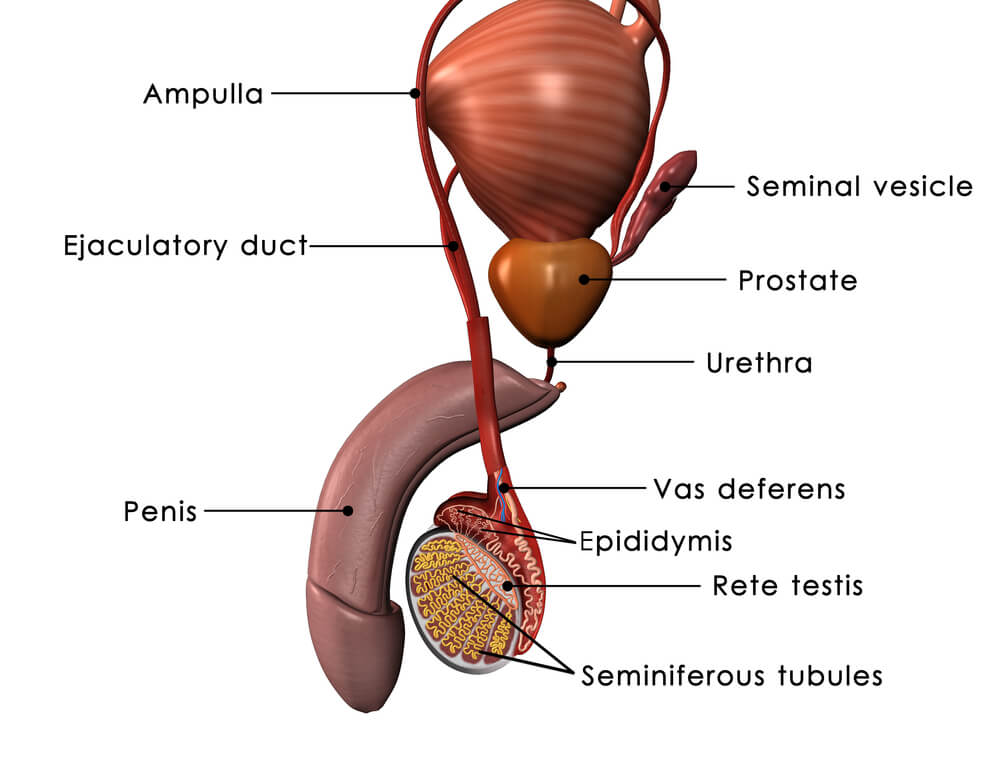
Seminal vesicle anatomy is a simple topic; after all, these glands only have one function – to produce seminal plasma. Seminal vesicle location is between the fundus (underside) of the bladder and the rectum and behind the prostate gland. You can see the location of (one) seminal gland in the image below. The other – if illustrated – would be very close to it, but to the left. Seminal glands open into ejaculatory ducts that are widened sections of the left and right vas deferens called the ampullae of the ductus.
The term vasa deferentia describes a pair of long tubes that transport spermatozoa and seminal plasma or components of seminal plasma from the left and right testes, via the epididymides (plural of epididymis), and out of the urethra. A single tube is called a vas deferens.
Before these thin, hollow tubes reach the prostate gland, they link to the right and left bulbourethral glands (Cowper’s glands). Cowper’s glands secrete a thick, alkaline fluid. When the vasa deferentia travel through the center of the prostate gland, each widens to form the ampulla of the ductus. It is here that the seminal glands empty their contents. Each vas deferens ends inside the prostate gland, where both empty into the single urethra. In the image below, the larger rounded structure at the top is the bladder.
Seminal vesicle histology – cell and tissue type – reveals three distinct layers – a pseudostratified columnar epithelium lining (mucosa), longitudinal and circular muscle layer, and a layer of connective tissue. The muscle layers are important as, when they are triggered by the sympathetic nervous system, the muscles contract and propel seminal fluid out of the glands and into the vas deferens. The wider portions of the vasa deferentia at the ampullae of the ductus can cope with sudden, quite large quantities of seminal plasma and they stop this fluid from traveling backwards into the glands.
The pseudostratified columnar epithelium has many goblet cells that secrete mucins. These mucins make it easier for sperm to use their tails to propel themselves forwards. Pseudostratified columnar epithelium cells grow in height according to the presence and production of the hormone testosterone; if a man has low levels of testosterone, this epithelium layer shrinks and any seminal fluid produced will be low quality. Low quality seminal plasma can lead to fertility problems just as much as low quality sperm or low sperm counts.
Seminal Fluid
Seminal fluid or semen is mostly manufactured in the seminal glands of human males; smaller quantities are produced in the primary male reproductive organs of the testes and epididymides and in the other two accessory glands. There are three accessory glands in human males and mammals that have seminal vesicles – these are the seminal, bulbourethral, and prostate glands.
Loosely speaking, the testes produce up to five percent of seminal fluid, the epididymides and prostate up to thirty percent, the bulbourethral glands less than one percent, and the seminal vesicles anywhere between sixty and seventy-five percent. While sperm cells are living cells, the fluid through which they move is a mixture of products that increases their chances of survival and success in finding and penetrating a female egg. All of the ingredients of seminal plasma are essential for reproduction.

The components of seminal plasma are produced throughout the male reproductive system. The testes contain Sertoli cells that secrete spermatid carrier fluid, as well as Leydig cells that produce androgen (male) hormones. The epididymides located just above the testes add glycerol, immobilin, and quiescence factor. While glycerol protects the sperm cells, immobilin and quiescence factor stop them from moving and wasting energy before ejaculation.
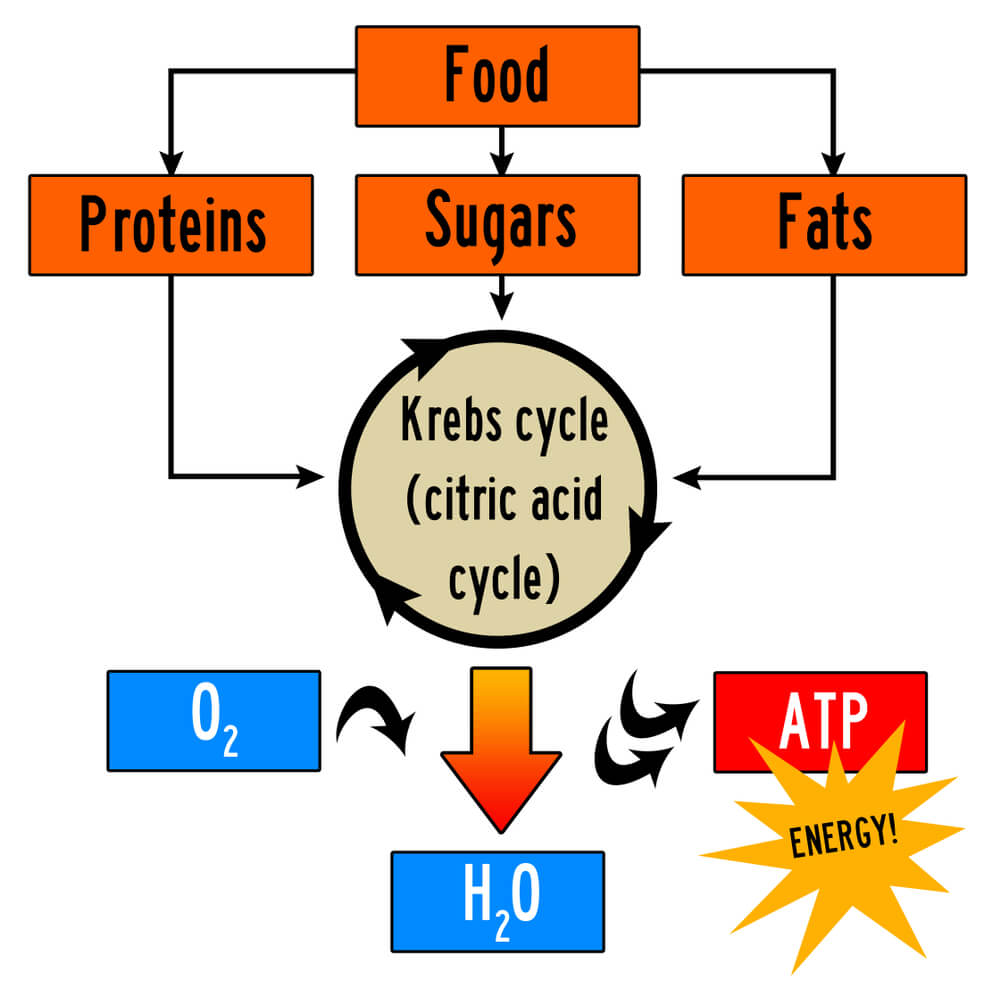
The ampulla of the ductus secretes ergothioneine that is though to act as an antioxidant, protecting the sperm from toxins. Alkaline mucus produced in each bulbourethral gland increases sperm motility and lowers the acidity of seminal fluid. This is important as the female reproductive tract is notoriously acidic. Before the addition of prostate fluid, the seminal vesicles add motility-helping mucoids, energy sources like sugars and citric acid, and protective factors such as ergothioneine. Citric acid is an essential organic acid that converts carbohydrates, lipids, and proteins into energy.
As this thickened fluid passes the prostate gland during ejaculation, zinc, coagulants, water, citric acid (see the image below), and acid phosphatase are added; the final product is known as semen or seminal plasma.
Seminal Vesicle Pain
Seminal vesicle pain is usually the result of an infection of the male reproductive or urinary tracts. These infections are most commonly prostatitis, urethritis, and cystitis. As the male reproductive tract shares the urethra with the urinary system, infections easily spread. When bacteria enter the seminal glands, seminal vesiculitis or spermatocystitis is possible. A seminal vesicle abscess might be the result and ejaculate can be foul-smelling, thicker than normal (pus), and yellowish. Seminal vesicle abscesses are more common after surgery, in diabetics, and in those who require urinary catheters over a longer period. Any untreated urinary or reproductive system infection can lead to permanent infertility.

Seminal vesicle inflammation means that the essential ingredients of seminal plasma become imbalanced. Any type of male reproductive or urinary tract infection can, when untreated, lower the chance of successful reproduction by affecting sperm nutrition, motility, and immunity. The treatment of seminal gland infection usually requires antibiotics.
If a benign (noncancerous) seminal vesicle cyst develops, a man might never know. As long as it stays small there are very few symptoms. Only when a cyst grows can it squash the seminal tract and cause localized pain, painful ejaculation, difficult urination, and often invisible blood in the semen. Seminal gland cysts are usually the result of narrowing (stenosis) in one vas deferens; this stops the affected seminal gland from draining properly. It becomes enlarged, inflamed and swollen. Most cysts are congenital and only found in one seminal vesicle.
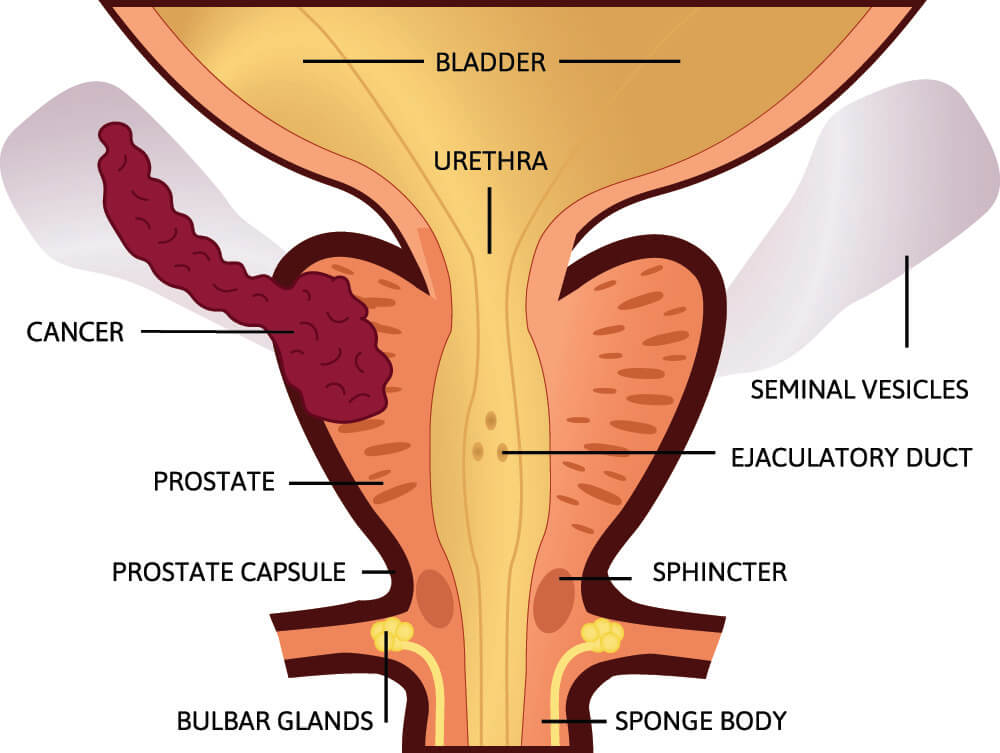
Seminal vesicle stones (calculi) are extremely rare. They form when a narrowed vas deferens causes seminal fluid to travel backwards into the gland. The seminal plasma stagnates and proteins and/or salts are given the opportunity to form crystals or stones. The very few and very rare seminal vesicle stones that have been examined are usually the result of protein build-up. Seminal gland stones cause obstruction and infection. If they cause a blockage in duct that exits the gland, seminal vesicle stones must be broken up using lithotripsy (ultrasonic shock waves directed through the skin) or be surgically removed. Seminal vesicle cancer is extremely rare unless it is the result of metastasis – spread from other cancers – that develop in close-lying structures like the prostate, bladder, or rectum.
Quiz
