Definition
Vasoconstriction is the narrowing or even closing of the lumen of a vein, artery, or arteriole as a result of smooth muscle cell constriction in the blood vessel wall. By reducing the diameter of a blood vessel, circulating blood must move through a smaller area under higher pressures. Vasoconstriction is regulated by the autonomic nervous system.
What is Vasoconstriction?
Vasoconstriction is the regulation of blood vessel diameter in the arteries, arterioles, and veins. It can be a life-saving reaction to sudden blood loss but can become harmful in the long-term. Vasoconstriction reduces the area volume inside blood vessel lumens.
Vasoconstriction affects vascular tone. Vascular tone describes how dilated or constricted the walls of a blood vessel are. Whenever we talk about vasoconstriction and vasodilation we are not including the capillaries – capillaries have no muscular walls and cannot constrict or dilate.
Many feedback systems control vascular tone. Extrinsic factors secreted by areas of the body far from the target blood vessels or organs, and intrinsic factors from the blood vessel or its surrounding tissues alter the systemic vascular resistance.
Systemic vascular resistance (SVR) is the total resistance to blood flow in all blood vessels except those in the lungs. Vasoconstriction increases systemic vascular resistance; vasodilation lowers it.
Pulmonary vascular resistance only describes the vascular tone of the arteries and arterioles that bring deoxygenated blood to the lungs. These vessels do not have significant wall musculature because to constrict the blood vessels of the lungs would mean low oxygen levels throughout the body. This is why systemic vascular resistance and pulmonary vascular resistance are two different things. This article will concentrate on systemic vascular tone.
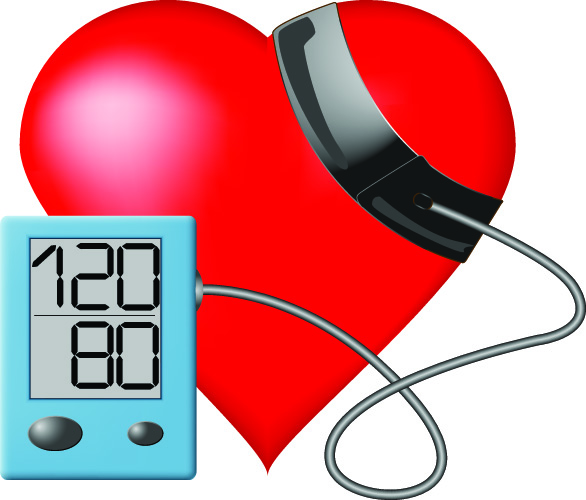
Vasoconstriction is a negative feedback loop reaction to hypotension or low blood pressure. Systolic pressure is the pressure that pushes on the artery walls when the ventricles contract (systole). Normal systolic pressure is around 120 mmHg.
When the heart muscle relaxes, the pressure on the artery walls is called diastolic pressure – the lowest pressure in the measured artery. On average, this value is 80 mmHg. The typical 120/80 blood pressure gives the systolic and diastolic values.
While occasional low and high blood pressure readings are not uncommon and are necessary to optimize blood flow, continuous lows and highs (chronic) can be harmful. Constantly abnormal blood pressure results often indicate serious pathologies.

Vasodilation and Vasoconstriction
Vasodilation and vasoconstriction work hand-in-hand. They are regulated by various genes and feedback mechanisms. While vasoconstriction usually occurs in the presence of low blood pressure, vasodilation can be the result of hypoxia (low oxygen levels), nutrient starvation, hyperthermia, and hormone imbalance.
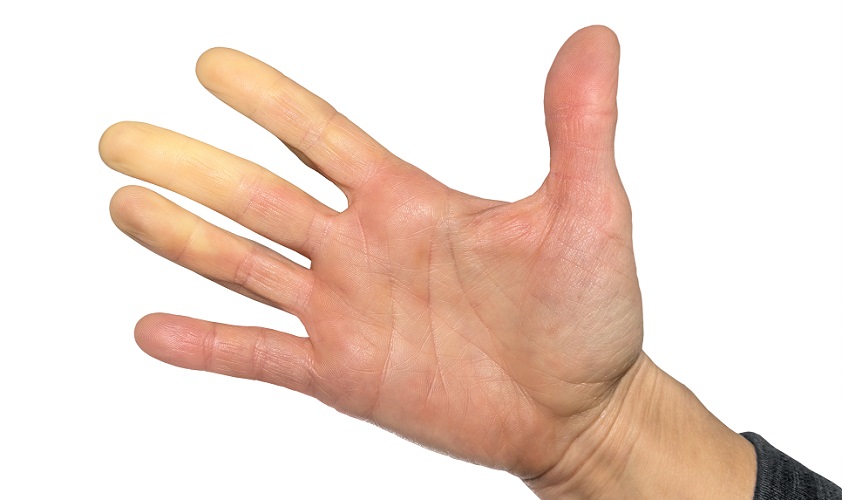
When blood vessels dilate the blood pressure becomes lower; the volume of space created by the countless lumens increases. When the weather is warm, we become flushed and may feel a little faint. The blood vessels in our skin dilate so that heat can radiate out from the body and lower the internal body temperature. The vascular tone decreases and it is possible that – for a short time – insufficient oxygen and nutrients (glucose) reach the brain. This makes us feel unsteady on our feet but in more severe cases can cause unconsciousness.
If left untreated, and if a person remains in a warm environment, heat stroke can be fatal.

The triggers for vasoconstriction are fluid loss (blood, urine, stomach contents, sweat, fluid evaporation due to severe burns), hypothermia, and hypernatremia (too much sodium in the blood). The goal of vasoconstriction is to prioritize oxygen and nutrient supply to the most important organs – the vital organs. Shock reactions caused by allergies, severe blood loss, major infections, heart disorders, hypoglycemia (low blood sugar), or thrombosis (blood clots) all stimulate vasoconstriction because these triggers are all life-threatening.
By shunting blood away from less vital organs like the skin and digestive system and instead sending it toward the lungs, heart, kidneys, brain, and liver, the chances of survival are increased.
When peripheral blood vessels constrict those of the vital organs dilate. As the vessels in the lungs are nearly always dilated, the effect here is less than in the other four vital organs. Vasoconstriction does not occur all over the body at the same time – it always works together with vasodilation.
Vasoconstriction Causes
Many causes of vasoconstriction have already been mentioned but the complete feedback system is quite complex.
Vasoconstriction causes can be classified according to pathology, organ or tissue type, specific environments, and mechanisms. Each category is a separate entity that causes a similar effect – the narrowing of a group of blood vessels.
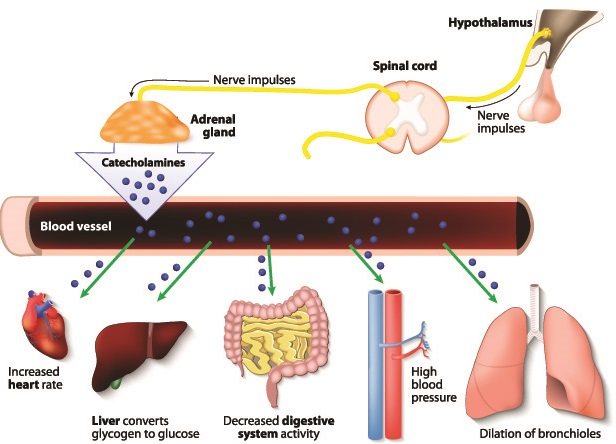
Endogenous vasoconstriction is regulated by the sympathetic (fight/flight) nervous system. Each muscular artery, vein, arteriole, and venule wall is in direct contact with sympathetic nerve fibers which signal them to constrict or dilate (relax) according to the neuron firing rate.
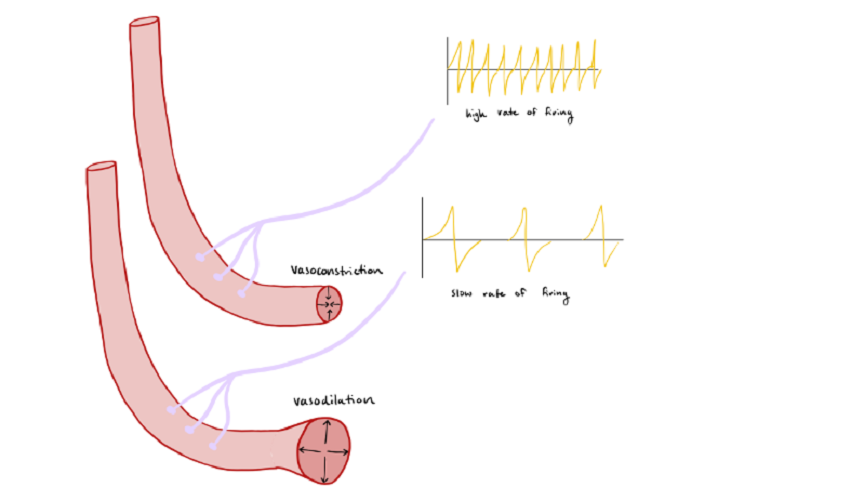
The diameter of a blood vessel lumen is controlled by the sympathetic noradrenergic vasoconstrictor system and the non-noradrenergic vasodilator (relaxation) system. Noradrenergic means that the nerve pathway responds to the neurotransmitter and hormone noradrenaline (norepinephrine). The vasodilation mechanism does not respond to this neurotransmitter.
The vasodilatory system does not increase lumen size beyond resting state. In other words, a blood vessel does not expand but either constricts or returns to its original shape. When triggered, the sympathetic nervous system increases its activity in the sympathetic noradrenergic vasoconstrictor system. This activity overrides the non-noradrenergic vasodilator system signals that keep blood vessel muscles in their natural, relaxed (dilated) state.
This explains why loco-regional anesthetics like nerve plexus blocks cause flushing in the anesthetized area; both the sympathetic and parasympathetic nerves are shut off. Without any stimulation the blood vessels in the anesthetized area are at rest – dilated.

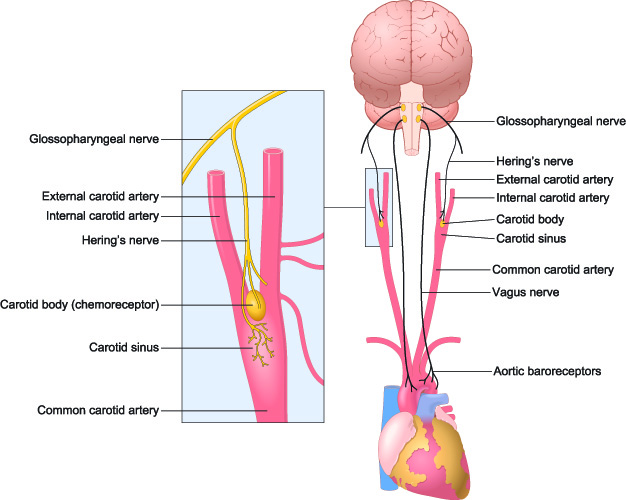
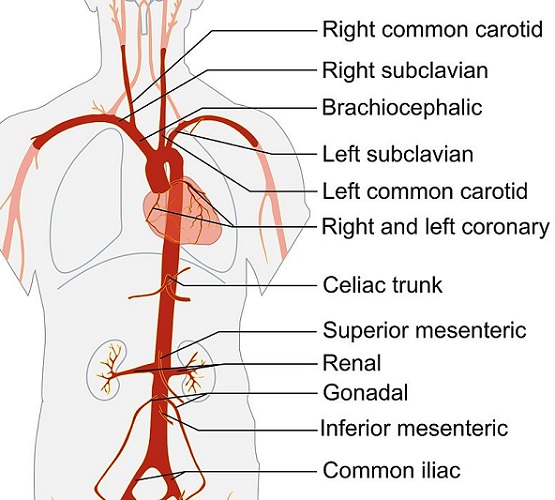
Another cause of vasoconstriction is the action of stretch-sensitive mechanoreceptors (baroreceptors) found primarily in the arch of the aorta and the carotid arteries (see below). Baroreceptors respond to changes in the diameter of these vessels.
When higher blood flow causes the elastic fibers in the vessel walls to stretch, rapid signals are sent which override and inhibit the firing rates of the sympathetic nerves. If blood flow is low and no stretching is detected, the baroreceptor signals slow down. This slower rate does not override or inhibit the sympathetic nervous system. With sympathetic signals being dominant, the blood vessel walls constrict. In short, rapidly firing baroreceptor signals override sympathetic nerve fiber firings.
Neurotransmitters also cause vasoconstriction. Alpha-adrenergic receptors are stimulated by noradrenaline, as are all of the receptors of the four types of heart activity:
- inotropic (force of heart muscle contraction)
- chronotropic (rate of heart muscle contraction)
- bathmotropic (how much the heart nerve tissue responds to stimuli)
- dromotropic (conduction of these stimuli).
Alpha-adrenergic receptors change the systemic vascular resistance by stimulating vasoconstriction. Alpha-adrenergic receptors in the kidneys, skin, intestines, and liver can also cause vasoconstriction.
Vasodilation is regulated through beta-adrenergic receptors in skeletal muscle.
Yet another cause of vasoconstriction is the renin-angiotensin-aldosterone system (RAAS) that regulates blood pressure and is continuously active. This feedback system is supported by sympathetic nerve activity in the kidneys. The kidneys will filter out less fluids in response to low blood pressure.
Whenever hypovolemia is detected, the kidneys stimulate alpha-adrenergic receptors on their localized blood vessels. Renal nerves then increase the release of renin.
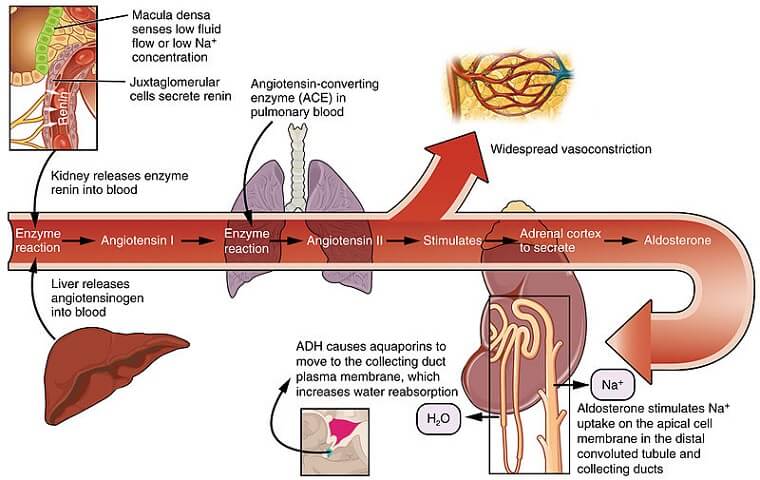
Renin converts angiotensinogen into angiotensin I, which is converted into angiotensin II with the aid of angiotensin-converting enzyme (ACE). Angiotensin II increases production of the hormone vasopressin (antidiuretic hormone) and also stimulates vasoconstriction receptors. Vasopressin works specifically on the arterioles (smaller arteries) and can rapidly raise the blood pressure when blood or fluid loss is not extensive.
Even cells in the inner lining of blood vessels play a role in vasoconstriction. The endothelium helps to adjust vessel tone, primarily in the kidneys. Endothelial cells release a hormone called endothelin. Higher levels of endothelin are found in heart, stroke and cancer patients, and also in people with metabolic disorders such as diabetes.
Endothelin is produced when blood platelets are required to travel to a wound. It is produced in higher quantities in the presence of toxins, thrombin, insulin, hypoxia, and the natural vasoconstrictor hormone vasopressin.
Specific Organ or Tissue Vasoconstriction
Vasoconstriction does not occur throughout the entire body at any one time. On the contrary, only the most crucial organs are protected from low blood pressure. Vasoconstriction in blood vessels that bring blood to the vital organs would prevent these organs from getting enough oxygen and nutrients. The mechanism also inhibits the removal of waste products such as carbon dioxide.
This explains why it is important that blood vessels in specific tissue groups react differently across the body.
Vasoconstriction in the Brain
A decrease in cerebral artery carbon dioxide levels causes vasoconstriction in the cerebrum; however, high oxygen pressure in these arteries does not cause vasoconstriction. This is a protective mechanism and ensures a continuous oxygen supply of blood to the brain.
Cerebral vasoconstriction can be the result of the rare reversible cerebral vasoconstriction syndrome (RCVS), associated with severe headaches caused by lack of oxygen as the arteries of the brain narrow. RCVS causes sudden, extremely painful headaches and even seizures as parts of the brain no longer get enough oxygen or nutrients. These headaches recur over days or weeks and then disappear. They are triggered by physical exertion or extreme stress.

Vasoconstriction in the Kidneys
In the kidneys, blood pressure levels are controlled by a myogenic (initiated by the muscle) mechanism and not directly by the sympathetic nerves. This means that even in cases of severe blood loss, the kidney still receives a blood supply – at least temporarily.
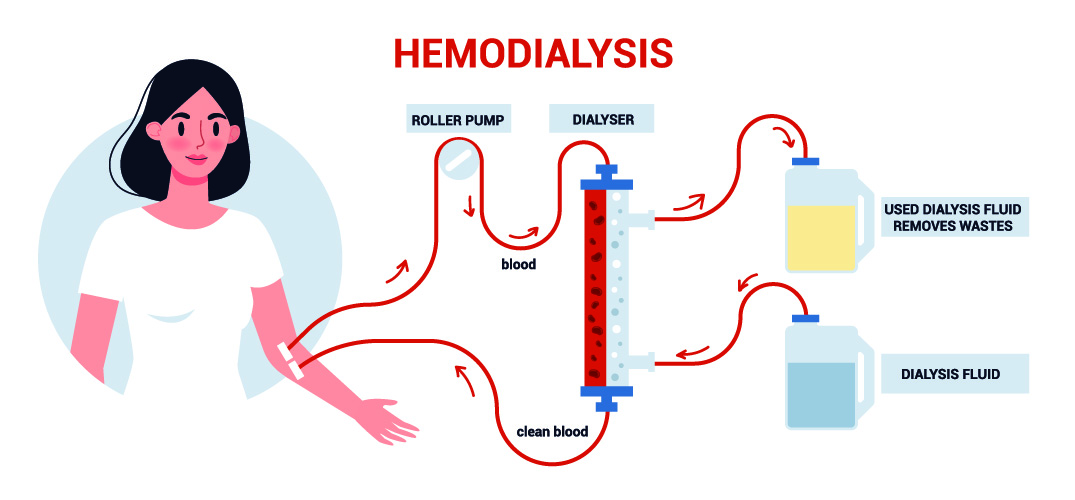
Severe fluid loss will eventually lead to the arterioles within and surrounding the kidney to constrict, severely affecting kidney function. As a vital organ, acute kidney failure can be fatal without immediate treatment. Patients will need hemodialysis to remove the toxins and excess minerals and sugars that the kidneys usually filter into urine.
Vasoconstriction in the Lungs
The lungs are responsible for oxygen supply and carbon dioxide disposal. It is logical that the lungs respond differently to low blood pressure or lack of oxygen. When an area of low oxygen is detected in the lungs, vasoconstriction will only occur in the areas with the lowest levels of oxygen, shutting them off. Blood is then directed to the properly functioning areas.
Vasoconstriction in Skeletal Muscle
During exercise, skeletal muscle requires a lot of oxygen and energy. As skeletal muscle contains a large proportion of the body’s blood vessels, this system also has its own set of vasoconstriction mechanisms.
When muscles are at rest they are not under the influence of hormones but are directly controlled by sympathetic activity. When at work, localized vasoconstriction occurs in muscle groups that are not working as hard, while the blood vessels within more active muscle groups dilate (relax).
Vasoconstriction in the Skin
Vasoconstriction mechanisms in the skin are purely under the influence of the sympathetic nervous system. This helps to alleviate extremes in temperature – a phenomenon known as thermoregulation.
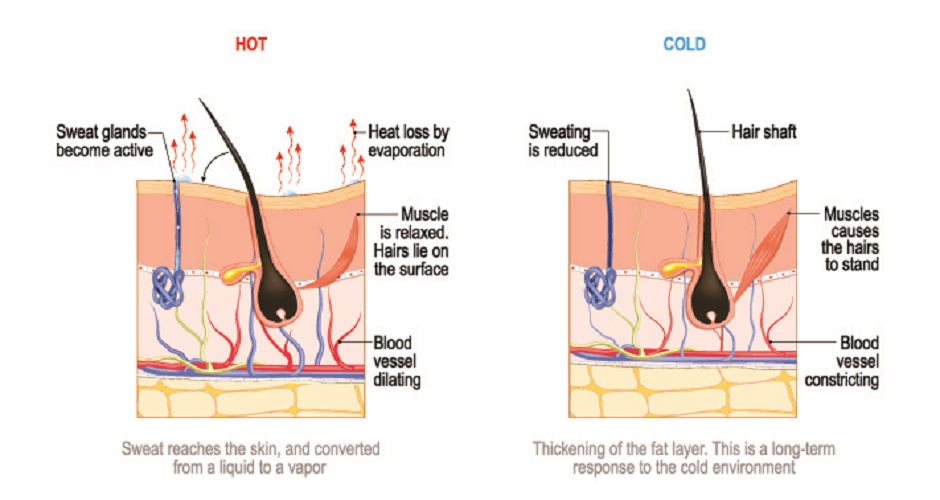
In warm temperatures, blood vessel dilation (relaxation) occurs due to an inhibited sympathetic response. When temperatures get low, this inhibition is reduced. You can adapt to temperature extremes over time, but otherwise any responses to ambient or internal temperature changes are very rapid.
Venous Vasoconstriction vs. Arterial Vasoconstriction
Veins are our blood reservoir, bringing blood back into the heart through the force of heart contraction. Valves inside the veins of the lower limbs work against the forces of gravity; otherwise whenever we stood still, our blood would rush to our feet.
Approximately 60% of the total blood volume is locate in the veins when the body is at rest. During physical exercise, venous vasoconstriction significantly increases the circulating blood volume, pushing its reservoir into the general circulation to feed the very hungry skeletal muscles.
To fully understand this mechanism, one first needs to understand the Frank-Starling law.
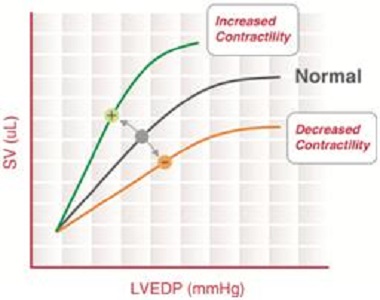
The above image shows the foundation of this law. You can see how the curve of heart muscle contraction gradually levels. Stroke volume (SV) is represented in the vertical axis and left ventricular end-diastolic pressure (LVEDP) in the horizontal axis.
All curves level off. This is because the heart is limited in how far it can contract. When the stroke volume is high, the heart contracts more strongly and the pressures that push blood from the heart into the aorta become greater.
The Frank-Starling Law
The more the ventricles of the heart stretch outwards when filling with blood the more they fill. The more they fill, the stronger they contract. And the stronger the ventricles contract, the better the circulatory flow and the more the tissues of the body are oxygenated and fed.
But ventricles cannot stretch without limit. Also, strong contractions are not always efficient as they use more energy. The heart must constantly adjust how hard it contracts.
How the heart adjusts these contraction forces and pumped blood volumes is explained by the Frank-Starling mechanism. Where this blood arrives and which organs or tissues take priority is regulated by vasoconstriction and vasodilation.
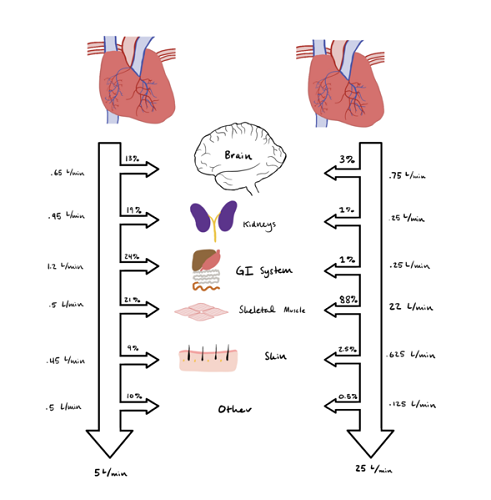
The below image shows approximately how much blood is pumped through the body during exercise (right-hand column) and at rest (left-hand column). As you can see, when we are exercising our skeletal muscle requires a huge amount of blood. The Frank Starling mechanism makes the heart muscle contract more strongly to achieve this – this is why many heart attacks occur during exercise.
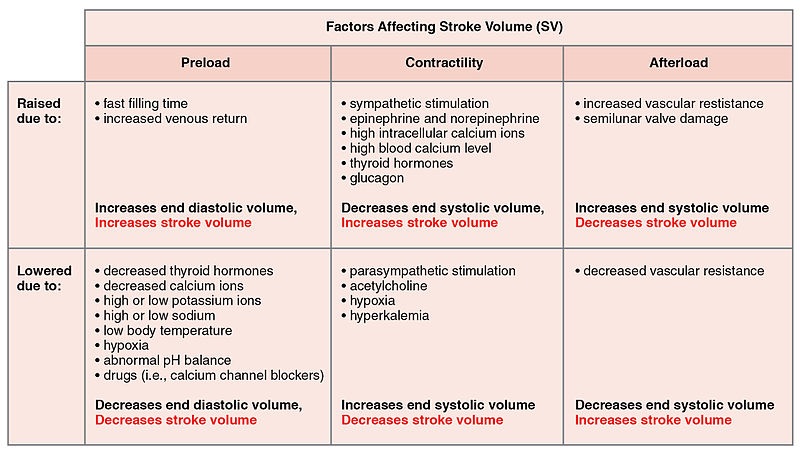
Stroke volume is the amount of blood the left ventricle pumps into the aorta every time it contracts. The larger the person, the larger the stroke volume, unless the heart is damaged.
The stroke volume (in ml) multiplied by the per-minute heart rate is the cardiac output – a value measured in liters per minute. Size matters, and weight in kilograms is also taken into account.
The average, at-rest cardiac output of an athletic young female with a heart rate of 58 bpm and weighing 120 lb. (55kg) is 3,250 ml or 3.25 liters per minute. An overweight, sedentary male of 220 lbs. (100 kg) with a resting heartbeat of 70 beats per minute would have a cardiac output of approximately 7 L/m. This higher figure leads to hyperdynamic circulation (too large quantities of blood passing through the heart) and an enlarged heart which will not function efficiently.
Whenever the heart beats more rapidly or slowly, or when the heart contracts more or less forcefully, the cardiac output changes. This occurs by way of the Frank-Starling mechanism, that changes the cardiac output according to arterial blood supply and venous return.
Frank-Starling and Venous Pressure
When we stand from a sitting position, our cardiac output drops. This may seem strange, as movement usually increases the heart rate and heart contractility. However, the action of standing causes blood to fall rapidly downwards (by way of gravity) to the veins of the lower body. The result is a sudden drop in blood pressure and a lower volume of blood enters the heart. The increased heart rate is a result of this pressure drop.
When this sudden fall in pressure results in fainting or dizziness it is called orthostatic hypotension. Orthostatic hypotension is a relatively common disorder in the elderly, where physiological responses work less efficiently. It is even thought that, as humans did not begin to walk on two legs until quite late in their evolutionary process, human genes have not yet had enough time to adapt to the upright position.

Less blood entering the heart means that the heart does not expand as much and will not contract as strongly (Frank-Starling’s law). As we have learned, this means a lower cardiac output. To compensate, the heart rate must increase. However, a further way and extremely effective way to increase cardiac output is vasoconstriction.
Pulse Pressure
Chronic high resistance (loss of elasticity) in the arterioles, usually due to atherosclerosis and aging, can lead to high pulse pressure. Pulse pressure is the difference between systolic and diastolic pressure. The ‘perfect’ blood pressure of 120 mm Hg systolic and 80 mm Hg diastolic has a pulse pressure of 40 mm Hg (120 minus 40).
A healthy pulse pressure is at least 25% of the systolic value. Anything lower than this is a narrow pulse pressure, usually seen in patients with severe blood loss or in people with heart failure. A narrow pulse pressure indicates a low stroke volume, which we now know leads to reduced cardiac output. In response, the peripheral blood vessels constrict and the heart rate increases.

Extreme sport brings this situation to the other end of the spectrum, causing wide pulse pressures. In healthy individuals, a higher stroke volume brings more oxygen and nutrients to the muscles. The same effect can be caused by high arterial resistance (chronic vasoconstriction). However, long-term wide pulse pressure does not necessarily mean you are fit and healthy; it can cause heart, brain and kidney damage.
Blood Vessel Compliance
Arterial, arteriole and venous walls must be compliant – flexible and elastic. Elasticity enables them to transport larger volumes of blood when required and constrict when blood needs to be shunted to vital organs. This degree in which a vessel is phyically able to relax and contract is known as compliance.
Atherosclerosis, faulty vasodilatory nerve circuitry, and the inability of the blood vessel walls to return to an original resting position can all lower compliance.
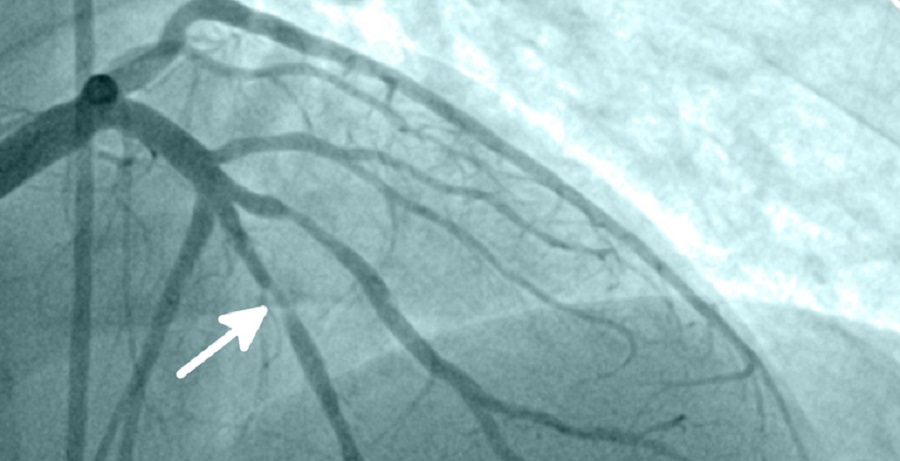
Rigid blood vessels caused by fatty deposits and localized inflammation (atherosclerosis) prevent larger volumes of blood from flowing through the circulatory system. This affects the transportation of oxygen and nutrients through the body and over time will cause organs to malfunction and wounds and tissue damage to heal much more slowly.
With thinner walls than arteries, veins are usually more compliant. They are more likely to be ‘too’ compliant. Varicose veins are the result of pooled blood distending the veins beyond their level of compliance. They can no longer return to their original shape. This is a little like a balloon that has been blown up much larger than it should and then deflated. Varicose veins present as thick, blue-colored bulges under the skin – most commonly in the calves.

In arteries, the lower the compliance the higher the systolic blood pressure and the more turbulence there is. Turbulence in the circulatory system can lead to the formation of blood clots that have the potential to travel to the lungs (pulmonary embolism) and brain (stroke), blocking off the blood supply. The heart must constantly work harder to overcome low levels of compliance.
Smooth muscle and elastic fibers of the arteriole wall contract or relax to regulate blood flow in specific areas of tissue. Arterioles do not need to cope with the high pressures that occur in larger arteries like the aorta, whose primary role is to push blood under pressure through smaller arteries and arterioles and into the capillaries. However, arterioles do need to regulate blood flow into the capillaries – a too high pressure could damage the delicate vessels and too low pressures will reduce gas, nutrient, and waste transport.
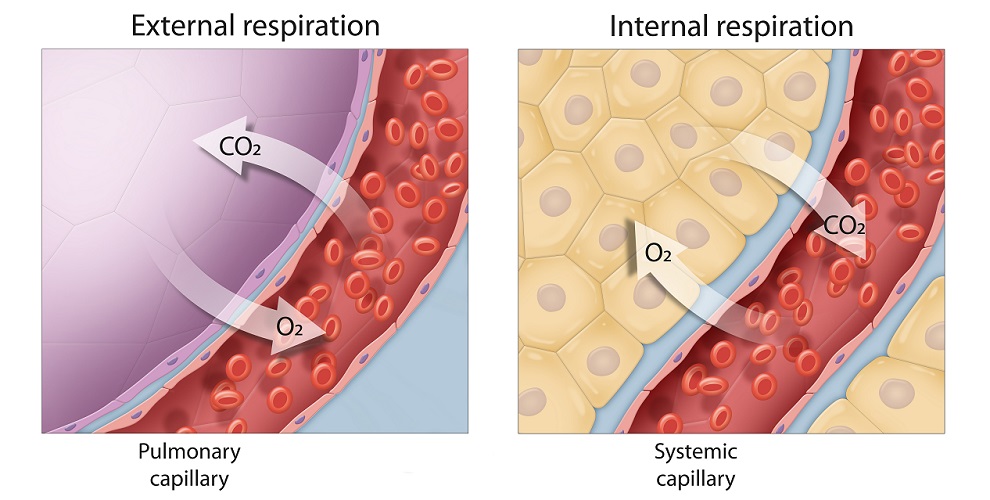
Only in the capillaries can oxygen and carbon dioxide exchange take place, and only in the capillaries can nutrient and waste molecules pass through their single-celled walls.
Finally, when considering blood vessel wall responses, if the elasticity of any blood vessel wall is compromised it will not react properly to signals from the autonomic nervous system. Vasoconstriction and vasodilation responses are much less efficient in people with low blood vessel compliance.
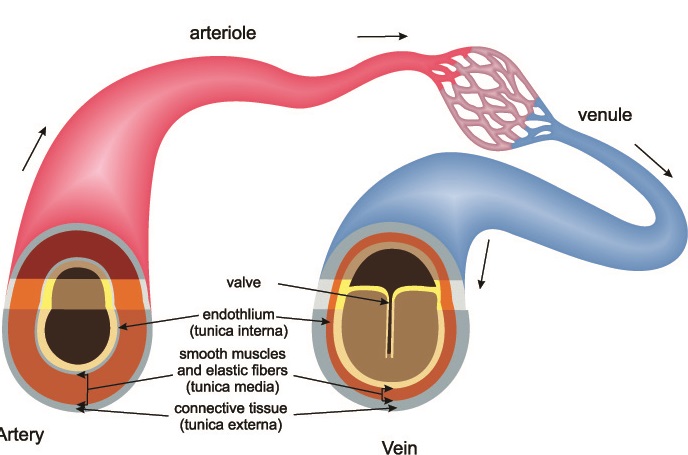
Arteries, Arterioles, Venules, and Veins
Arteries, arterioles, venules, and veins have different structures and functions. In the systemic circulatory system, arteries and arterioles bring oxygenated blood to the capillaries. Oxygen and nutrients can only diffuse into the surrounding tissues through the thin walls of the capillaries. Capillaries end at venules that transport the now deoxygenated blood (red arrows) into larger veins. The largest veins feed into the heart (vena cavae). The heart pumps this blood into the lungs where it once again becomes oxygenated (blue arrows).
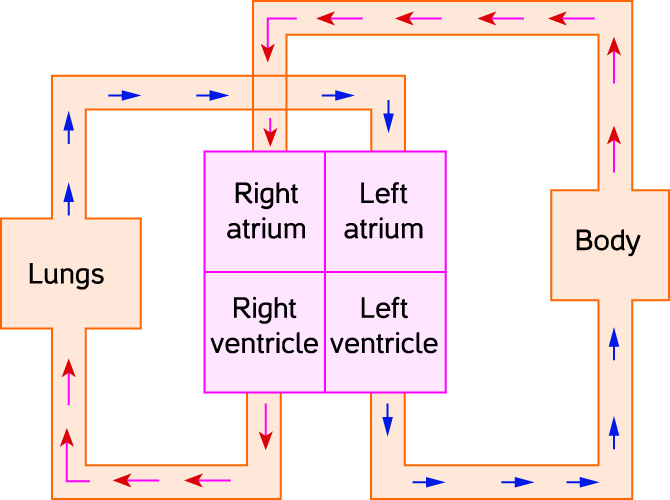
In the pulmonary system it is the pulmonary arteries that bring deoxygenated blood via arterioles into the lungs. Carbon dioxide is exchanged for oxygen and the pulmonary veins bring the newly oxygenated blood to the heart. In the rest of the body, arteries bring oxygenated blood and veins transport deoxygenated blood; in the pulmonary circulation this is the opposite.

Blood Vessel Structure
All blood vessels, apart from the capillaries, have similar layers. The outer layer of connective tissue – mainly collagen – is called the tunica adventitia or tunica externa. This layer contains a vascular nerve network (nervi vasorum); some larger veins and arteries also have vasa vasorum – tiny blood vessels that feed the muscular vessel walls.
Moving towards the lumen, the next layer is the tunica media composed of smooth muscle, connective tissue, and elastic fibers. This is where vasoconstriction takes place. Every artery and arteriole has an extra elastic membrane within the tunica intima. Large arteries have a significantly thicker tunica media. This thicker wall explains why arteries are much more likely to keep their rounded form when under external pressure, while a vein can be easily flattened, for example by an ultrasound probe.
The next layer is an elastic membrane that separates the tunica media from the tunica intima – a layer of cells and connective tissue (subendothelia) that supports a single layer of endothelium cells. Large arteries may have more than one layer.
The lumen is the hollow region of the blood vessel tube. Some veins have valves within their lumens – thin sheets of tissue that only allow blood to travel against the force of gravity under the influence of pressure supplied by the heart and arteries. Arteries and arterioles do not have valves.
Veins and Venules
Large veins are also composed of the abovementioned tunica layers, but the tunica externa also contains smooth muscle cells, vasa vasorum, and nervi vasorum.

In veins the tunica media is much thinner but, unlike the artery, also hosts the vasa vasorum and nervi vasorum. Lower pressure within the veins compared to the high pressures within the arteries means these layers will not be impaired when cardiac output is high.
Veins deal with return blood flow and do not experience high pressures (in healthy adults). In order to bring more blood back to the heart, venous lumens are usually larger in diameter. For example, the diameter of the lumen of a healthy ascending aorta is just under two centimeters. The diameter of the vena cava where it reaches the heart can reach three centimeters. The lumen of a vein may also contain valves. Finally, veins do not have an internal elastic membrane.
The difference between a vein and the much smaller venule is primarily to do with size. The same layers prevent diffusion into the lumen from the surrounding tissues – this only occurs in the capillaries. A vein feeds into multiple venules which feed into thousands of capillaries. We need lots of veins and venules to provide a readily-available reservoir of blood.
Arteries and Arterioles
There are two main types of large artery – elastic and muscular. The arteries closest to the heart are referred to as elastic (or conducting) arteries. They must be extremely compliant as they need to cope with the highest pressures as blood leaves the left ventricle. As conducting arteries are very close to the heart there is no vasa vasorum within the tunica externa; high intraluminal pressures supply enough oxygen to the vascular tissue. The tunica media is thickest in elastic arteries.
As the elastic arteries travel further from the heart they no longer need to deal with such high pressures and do not have to be so elastic. The tunica externa thickens and vasa vasorum and nervi vasorum appear. The tunica media of smaller arteries takes up less space in the arterial wall. They are called muscular arteries.
Arterioles are branches of muscular arteries (never of conducting arteries) that lead to capillaries. Arterioles have a thin tunica externa, a tunica media that is only one to two smooth muscle cells in width, and a tunica intima with endothelium and an elastic membrane.
Arterioles drastically slow the blood flow and are nearly always in a partially-constricted state. They are critical for blood pressure regulation as blood flows into the capillaries. Without the correct level of pressure in the thinly-layered capillaries, oxygen, carbon dioxide, nutrient, and waste exchange will not be efficient.
After gas diffusion has occurred, blood from the capillaries travels into venules. Veins and venules need wide lumens to store blood and sometimes contain valves. A larger lumen means thinner walls and overdistention is possible – varicose veins are the result of overdistantion or stretching past the normal limits.
When veins and venules constrict, blood returns rapidly to the heart.
Vasoconstriction and Migraine
Migraine, a subgroup of reversible cerebral vasoconstriction syndrome or RCVS, is the third most common global disease. It used to be thought that migraine was caused by enlarged cerebral and meningeal arteries.
Medications to treat migraine like rizatriptan benzoate work as vasoconstrictors, narrowing these enlarged vessels. Yet vasoconstriction can also be a trigger for migraine, especially when the body becomes accustomed to certain medicines or stimulants like caffeine. Not all migraine sufferers respond to vasopressor drugs. This has led researchers to look more carefully at other potential causes.
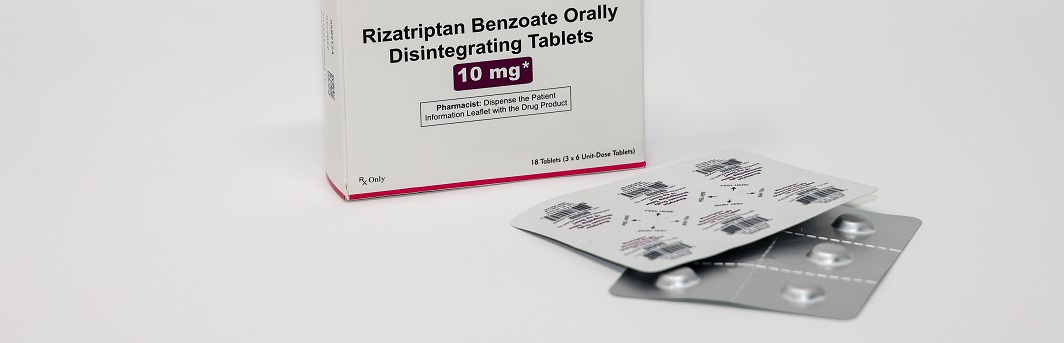
Vasoconstriction as the primary cause of migraine is now being strongly disputed. As migraines are much more common in women up until the menopause, sex hormones almost definitely play a role. Stress activates the hypothalamic-pituitary-adrenocortical axis that, among other things, releases stress hormones. The effects of these stress hormones (noradrenaline and cortisone, for example) affect vascular tone. Migraine could be a secondary symptom to stress. Additionally, excess serotonin is often found in the urine of migraine sufferers; its exact role is not yet clear.
As all endothelial cells seem to contribute to hormone and inflammatory processes, the large square area of blood vessels with their miles of endothelium make them much more than simple transport systems. The Franklin Institute tells us that, when stretched out in a single line, the blood vessels of a child would cover about 60,000 miles and those of an adult nearly double the distance. It is likely that blood vessels and vasoconstriction have many more effects that have not been discovered. In the light of this, migraine may also be the result of blood vessel anomalies and this often debilitating disorder certainly requires more complex therapy than vasopressor drugs.
Quiz