Definition
Serratia marcescens is an opportunistic gram-negative pathogen and one of the main Enterobacteriaceae responsible for hospital-acquired infections. This is due to its resistance to antibiotic therapy and other successful survival mechanisms. Previously thought to be non-pathogenic, S. marcescens became a recognized name when consciously used in U.S. military experiments in the 1940s and 1960s.

Where Is Serratia Marcescens Found?
Serratia marcescens is found in fresh and stagnant water or saline, in the soil, and in plants, insects, and animals including the human species. It has known pathogenicity for non-plant life made even more potent through its characteristic multi-antibiotic resistance.
S. marcescens can survive in biological and non-biological environments and has produced countless epidemics all over the globe. From contaminated water supplies to the passing on of a single bacterium in critical care wards, this bacterium’s ability to multiply in far from ideal conditions and its resistance to treatment means a Serratia infection is potentially fatal. From soil to crop to plate, or from healthcare worker to wound to the connective tissues of the central nervous system, highly motile Serratia bacteria are equipped to take every opportunity and colonize within a living organism.
A single-celled organism was discovered in the early 19th century after it was found to be the cause of polenta produced in an Italian village turn red. Yet historical evidence as far back as the 4th century A.D. describes the phenomenon of ‘bleeding bread’. This red coloration in certain food types was often associated with either divine or satanic intervention. In 1263, a Bohemian priest celebrated mass in Bolsena. As he bent over the sacramental wafer, it appeared to ooze blood, staining the altar. The Mass of Bolsena has been celebrated ever since, unwittingly praising the power of a microbe. While the Italian villagers, around 550 years later, believed this color change was due to satanic activity, scientists at the time realized the culprit was less miraculous and decided the reason for the bloody polenta was fungal in origin. They named this supposed fungus Serratia marcescens.

Serratia Marcescens Taxonomy
Serratia marcescens taxonomy remained a riddle up until the late 20th century. The first scientific papers described it as a stemless fungus. Later researchers believed it was yeast or mold. This led to multiple names for a single species of bacteria that further confused its study and postponed a final nomenclature until the 1960s.
S. marcescens is now accepted as a member of the Enterobacteriaceae order and a bacterium that, along with others within the Serratia genus, often produces a red pigment known as prodigiosin. It should be mentioned that not all pathogenic strains of Serratia produce this red coloration. Serratia marcescens is a gram-negative rod-shaped facultatively anaerobic bacterium that is extremely motile. An S. marcescens gram stain shows short, pink-colored dots, as seen below.

Rod-shaped bacteria, bacilliform bacteria or bacilli describe the typical shape of Serratia marcescens. This is a facultatively anaerobic microorganism, meaning it can grow in the presence or absence of oxygen, significantly increasing its chances of survival in various physiological systems. In addition, S. marcescens can grow in a wide spectrum of temperatures and pH levels, varying from the very acidic to the mid-alkaline.
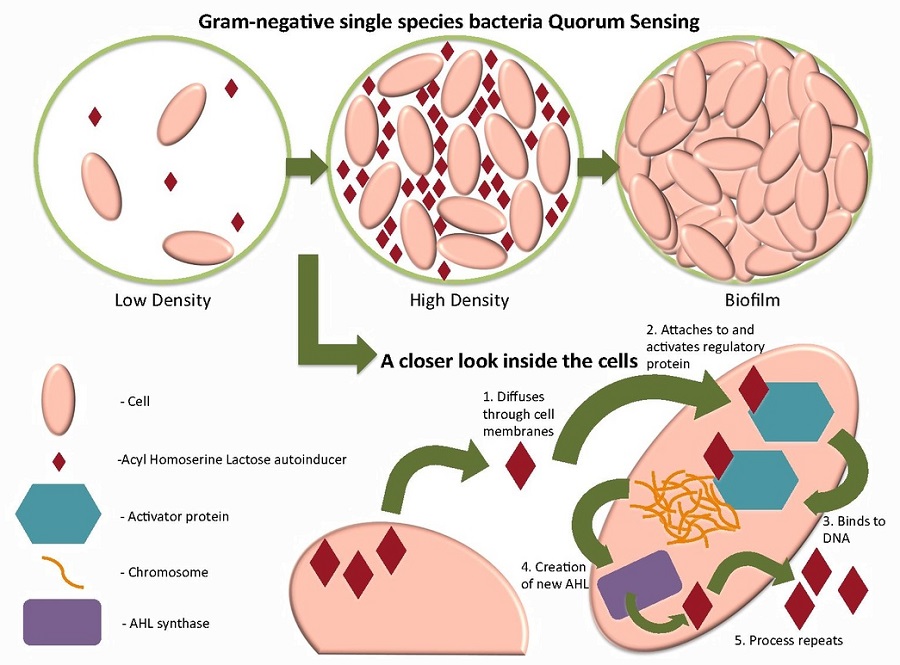
Serratia bacteria emit extracellular enzymes such as AmpC type β-lactamases, elastase, gelatinase, lecithinase, alkaline protease, and caseinase, all of which increase bacterial resistance to antimicrobial therapies. Communicating through channels within the biofilm – a type of cell signaling known as quorum sensing – all S. marcescens drug resistance factor (R-factor) characteristics within a single bacteria can be passed on to entire populations; it is also known that drug resistance in S. marcescens is significantly more prevalent than in other Enterobacteriaceae. What is more, transfer of R-factors between different strains of these bacteria is possible.
The final stage of biofilm formation – the dispersal stage – sends countless motile S. marcescens bacteria to other areas of the body and can be coughed, sneezed or excreted to infect others; however, the most commonly reported mode of transmission is healthcare worker hands.
Once created, an S. marcescens biofilm regularly sloughs away when its thickness has reached a certain height. This practically automated process allows multiple infection sites to form within a short period of time. In combination with resistance factors, this makes an S. marcescens infection potentially fatal in the critically-ill hospitalized patient.
Serratia Marcescens as a Tracer Organism
Serratia marcescens was used as a tracer organism for many years until its pathogenicity was finally revealed. In the First World War, where controlled medical experiments were often carried out on soldiers, the mechanisms of bacterial infection via the mouth and gastrointestinal system could be studied thanks to the distinctive red coloration provided by S. marcescens. Medical researchers would place S. marcescens on the gums before dental surgery to see whether bacteria could enter the bloodstream, for example. Most famously, the U.S. military used Serratia marcescens to show the results of possible biological warfare and released large numbers of Serratia into subway systems, government and military facilities, and entire urban populations. This led to infection and a small number of S. marcescens infection-related deaths. Press publicity of the ensuing court cases that began in the late 1960s reached global audiences.
Who Gets Serratia Marcescens Infections?
Outside of hospital settings, one may pick up a Serratia marcescens infection in countless ways, from the handling of coin currencies and non-disinfected countertops to infected crops or meat. Eye infections can be caused by infected contact lens and saline solutions; wound infections from improperly sterilized equipment or infected caregivers. Carried from hand to mouth or from fork to mouth, at least half of Enterobacteriaceae populations can survive in the highly acidic environment of the stomach. Once past the pyloric sphincter, they travel on into the less acidic gastrointestinal tract where they are given the opportunity to attach to the intestinal epithelium and multiply. The rapid development of a biofilm creates much improved S. marcescens living conditions and, in combination with antimicrobial drug resistance, easily causes infection in malnourished, elderly, very young or acutely and chronically ill populations. Healthy individuals can rely on natural immunity to keep Serratia populations under control.
As opportunistic bacteria within a clinical setting, S. marcescens infections usually only occur in immunologically-compromised patients, and in particular in intubated and catheterized elderly or very young patients. The overall mortality rate of S. marcescens infected patients in a hospital environment (and in combination with illness, advanced or young age or otherwise compromised immunity) is between 14% and 20%.
Why is Serratia Marcescens Hard to Eradicate?
Serratia marcescens is hard to eradicate due to the presence of antimicrobial resistance factors; this has already been discussed. However, other factors also play a role in Serratia’s survival both within the human body and without.
Where carbon and energy sources are limited – a situation referred to as carbon-starvation – non-sporing Enterobacteriaceae change their gene expression and so their physiology to survive in a near-dormant state for a significant amount of time. This is known as the starvation-stress response (SSR). S. marcescens has been shown to exhibit an even greater ability to withstand high temperatures, very low pH and oxidative stress even in a carbon starvation state. This phenomenon is known as starvation-induced cross-resistance and increases survival rates above and beyond those Enterobacteriaceae only able to exhibit SSR.
In addition, S. marcescens has a number of subspecies that differ in metabolism, virulence, and antimicrobial resistance. Through quorum sensing, all of these characteristics can be shared between different strains via the biofilm channels and according to the current environment. The following generations are subsequently more equipped to deal with stress within that environment, and much more difficult to eradicate.
S. marcescens is well known for its preference for moist surfaces and low-nutrient watery environments such as contact lens saline, improperly stored and contaminated intravenous saline, and breathing tubes on respiratory equipment that has not been changed for a period of time. Even in the absence of nutrients, these bacteria can survive. In addition, S. marcescens is extremely motile and can quickly transfer from a caregiver’s hands onto an exposed catheter or open wound.
When outside of a living organism, starvation-induced cross-resistance is at its most effective. Even powerful disinfectants may not eradicate Serratia strains. In fact, populations happily grow in disinfecting footbaths in swimming pools. You may even have noticed a slight pink tint to grout or silicone sealants in private or public bathrooms. This tint points to S. marcescens colonization.
In order to eradicate S. marcescens from countertops, bathrooms, medical equipment or any non-living surface, a 0.5% solution of Accelerated Hydrogen Peroxide (AHP) should be applied for a minimum of thirty seconds and anything between thirty seconds and five minutes to eradicate 99.999% (5-log reduction) to 99.9999% (6-log reduction) of Serratia bacteria. Very few cleaning teams are given the time to wipe every surface for half a minute, let alone five.
The best way to prevent passing on S. marcescens bacteria from person to person or from person to object is through thoroughly and correctly washing the hands (see below) with or without antiseptic. Rinsing the hands under running water causes large numbers of bacteria to be washed away and is often more effective than the incorrect use of hand sanitizers.

The ability of Serratia to survive in high temperatures is also of importance, as a high fever – an evolutionary mechanism to kill pathogenic bacteria within the body – does little to the presence of existing Serratia populations in comparison with other types of Enterobacteriaceae. In a carbon-starved state, this ability to survive in high temperatures is increased. Research shows that starvation-induced cross-resistance increases S. marcescens resistance to thermal, acid and oxidative stress. It is also understood that further stress response networks make this bacteria type one of the most virulent and resistant to biotic and abiotic factors that may control less resistant bacteria types.
Serratia Marcescens Symptoms
Serratia marcescens symptoms are multiple in the human species but most commonly associated with the species’ role in nosocomial infections such as catheter-associated bacteremia and respiratory system, urinary tract, and wound infections. In children, infections are usually limited to the gastrointestinal tract.
S. marcescens symptoms depend upon the localization of the infection and its spread. If an infected hand touches the eye and natural immunity is unable to fend off Serratia colonization, the result might be conjunctivitis, keratitis or tear duct infections, for example.
Once in the bloodstream, Serratia bacteria can cause endocarditis, bacteremia, meningitis, osteomyelitis and arthritis. Serratia marcescens treatment is limited to cefotaxime and gentamicin – both antibiotics. If Serratia strains develop resistance to these drugs, very few therapeutic options remain.
Serratia Marcescens as a Cancer Therapy?
Prodigiosin taken from strains of S. marcescens has been shown to be toxic to cancerous cells but much less so to non-cancerous ones. Because of this, prodigiosin is currently being studied as a natural medicine for cancer therapy. Cell toxicity – even to healthy cells – has always been a problem in the development of anticancer drugs. Microorganism metabolites such as prodigiosin – the pigment that produces the red coloration in S. marcescens colonies – inhibit certain cancer cell signaling pathways causing early cancer cell death; however, the exact action is not yet understood. Current studies have shown anticancerous activity of prodigiosin in breast cancer, prostate cancer, and choriocarcinoma although all of these studies took place in the laboratory. This area of study is known as bacteria-mediated cancer therapy or BMCT and is becoming increasingly popular as a pharmaceutical industry research topic.
Quiz
1. Which of these numbers represents a 5-log reduction?
A. 9999%
B. 99%
C. 9999 log
D. 999%
2. SSR refers to:
A. Starvation-stress cross-reference response
B. Starvation-survival response
C. Starvation-induced cross-resistance response
D. Starvation-stress response
3. What is BMTC?
A. A type of bacterial resistance to antimicrobial drugs
B. A pigment found in S. marcescens bacteria
C. Therapy for cancer using products produced by some single-celled microorganisms
D. A temperature-linked mechanism that increases bacterial survival in higher temperatures
