Definition
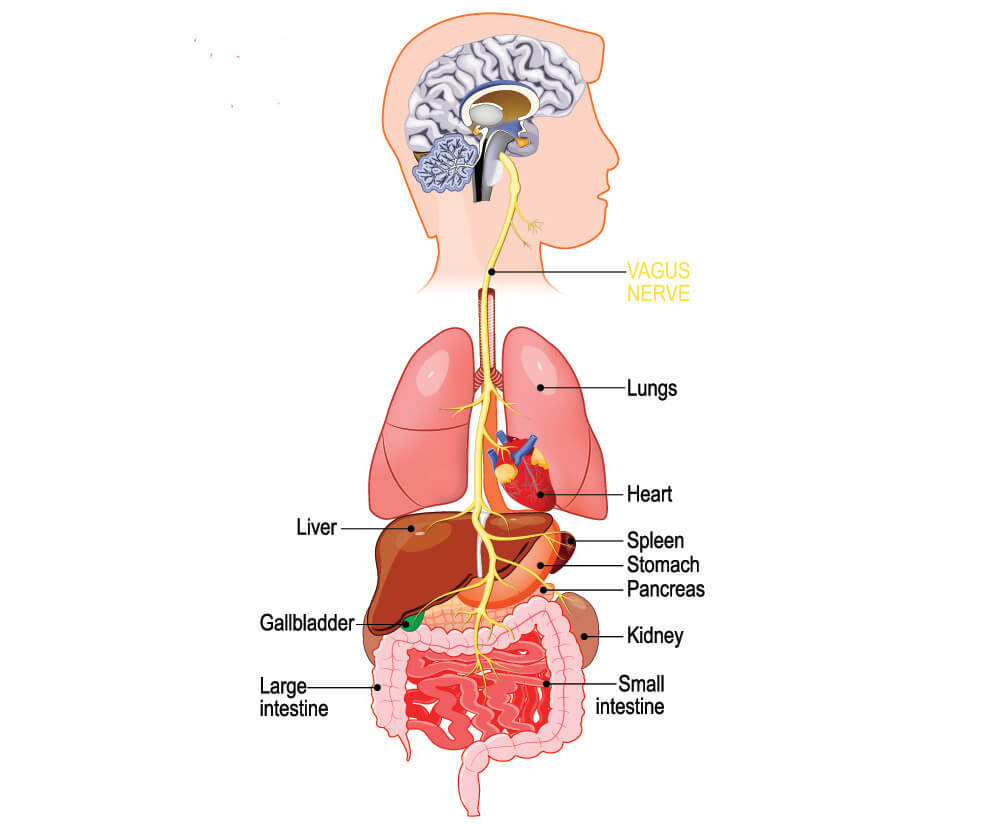
The vagus nerve is a mixed sensory and motor nerve with many functions that include immune response, heart rate, digestion, and mood control. As the longest of the cranial nerves, cranial nerve number ten (CN X) travels from the brain to the abdomen, also innervating parts of the face, throat, and thorax, and acting as a sensory, special sensory and motor nerve.
Vagus Nerve Function
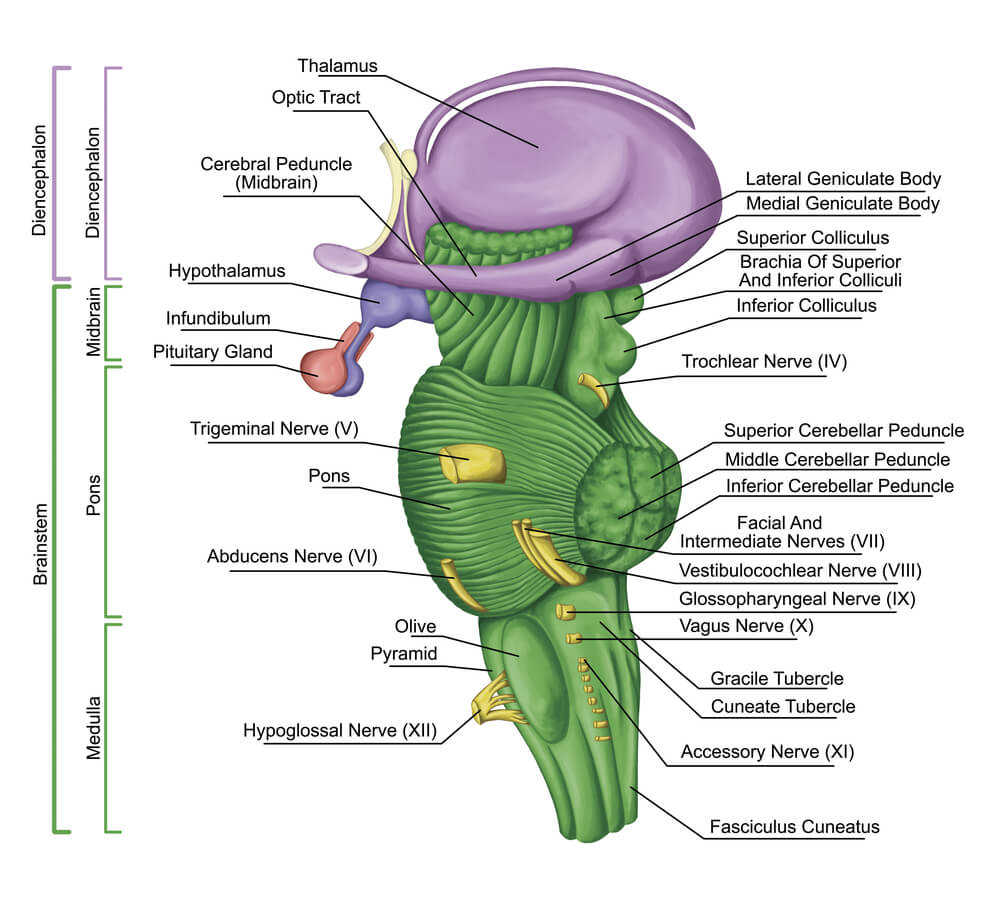
Vagus nerve function is split into four groups according to the type of nerve fiber: sensory, special sensory, motor, and parasympathetic. Although primarily an afferent nerve that brings sensory information from the body to the brain, the vagus nerve is also an efferent (motor) nerve that brings messages from the brain to muscle. Smooth muscle control is regulated within the parasympathetic nervous system. The vagus nerve originates in the medulla oblongata of the brainstem as you can see in the diagram below.
Four separate vagal pathways exit from the medulla oblongata:
- Dorsal nucleus: sends parasympathetic information to the viscera
- Solitary nucleus: receives sensory information from the tongue (taste) and visceral organs
- Spinal trigeminal nucleus; receives sensory information from the outer ear and laryngeal mucosa
- Ambiguous nucleus: motor nerve associated with speech, swallowing, and heart muscle activity.
Cranial nerve nuclei are collections of gray matter located in the brainstem and represent a point of synapse. Neurons exiting the vagus nerve in the medulla oblongata first synapse in their associated nuclei before continuing to different locations in the body; similarly, messages sent to the brain from other areas of the body synapse at the nuclei before their messages reach the medulla oblongata.
As a sensory nerve, CN X innervates the skin and mucous membranes of the external ear, throat (laryngopharynx), and voice-box (larynx). It also provides visceral sensation in the heart and visceral organs that allow a person to feel pain, distension, vibration, and nausea. The nerve also sends involuntary signals in response to specific chemical stimuli – neurotransmitters and hormones, for example. The visceral organs or viscera include the heart, lungs, liver, pancreas, and intestines.
As a special sensory nerve – where special describes the senses of smell, vision, taste, hearing, and proprioception – the vagus nerve collects information from the taste buds of the back of the tongue and upper epiglottis. As a motor nerve, CN X innervates the muscles of the throat.
The parasympathetic nervous system has an involuntary resting function that brings the body back to a calmer state after the sympathetic fight and flight reaction is no longer necessary for survival. The vagus nerve is part of the parasympathetic nervous system and innervates the smooth muscle of the heart, trachea, bronchi of the lungs, and gastrointestinal tract. If stimulated, it will make the heart rate and breathing rate slow, and increased gut peristalsis.
Vagus Nerve Stimulation
Vagus nerve stimulation is nothing new; vagal maneuvers have been used for centuries to lower the heart rate and induce a sense of relaxation. The ancient Greeks called the carotid artery the ‘site of sleep’ as – unbeknown to them – massage to this area stimulates the vagus nerve that lies alongside the much more visible and palpable artery. Massaging the right carotid region lowers the heart rate and blood pressure. Hippocrates made it very clear that every physician should be extremely adept in the art of ‘rubbing’.
In today’s medical world, the vagus nerve is stimulated using two methods. The first is a group of actions known as vagal maneuvers. The second is electrical stimulation of the vagus nerve.
Patients with supraventricular tachycardia suffer from a heart rhythm disorder associated with a suddenly-occurring rapid heart rate. Symptoms are palpitations, shortness of breath, lightheadedness, and sweating. While medications help, patients are also taught various vagal maneuvers as a first-line therapy that can often negate the need for a hospital visit. These actions include coughing, holding the breath, and splashing the face with icy water. Such activities temporarily increase intrathoracic pressure and in doing so, increase the blood pressure. In reaction to this artificial high blood pressure, the vagus nerve kicks in by slowing down the heart – a parasympathetic signal that also brings the blood pressure down. Cold water to the face also provokes the Diving reflex that results in a slower heart rate, a temporary holding of the breath, and the constriction of peripheral blood vessels that increases oxygen supply to the most important organs.
Other methods are also effective. Touching the back of the throat encourages the gag reflex which also stimulates the vagus nerve. Carotid massage just under the angle of the jaw is only done in patients without atherosclerosis as plaque can break off and cause a stroke. Carotid massage places immediate pressure (stimulation) on the cranial nerve X. This treatment should only ever be done by a medical professional.
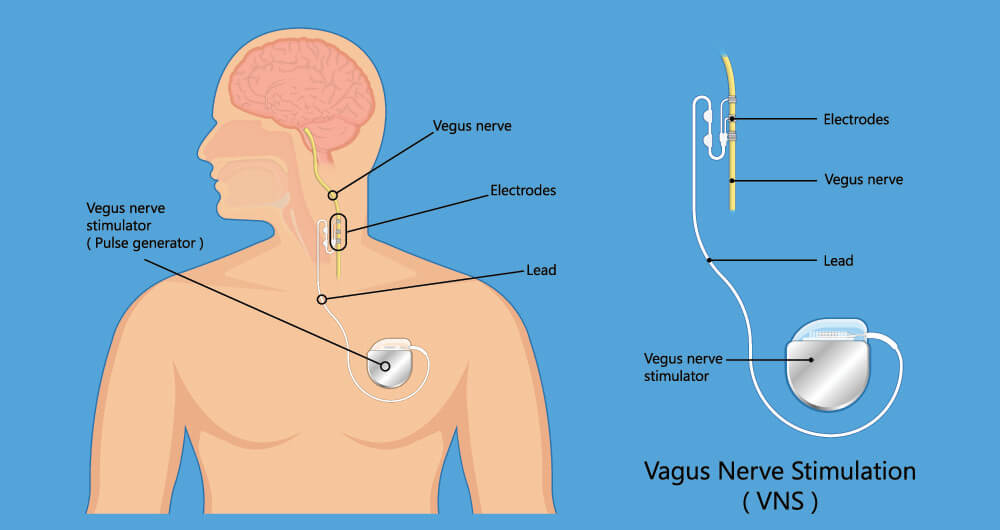
Electrical vagus nerve stimulation (VNS) uses electrical impulses applied to the nerve and these can be either be applied with an implanted device (see the image below) or be given as a portable, temporary therapy. While not all medical journal contributions agree that electrical vagal stimulation is worthwhile, many patients and physicians have seen improvements during and after VNS in the treatment of depression, multiple sclerosis, epilepsy, Alzheimer’s disease, metabolic syndrome, cardiovascular disorders, Parkinson’s disease, migraine, tinnitus (ringing in the ears); and cluster headaches. Newer, wireless devices are being developed to help people rehabilitate after a stroke.
Recently, a study about transcutaneous vagus nerve stimulation (tVNS) of the outer ear for fifteen minutes a dag increased cardiovascular health, mood, and sleep in the over 55s. But stimulation of the ear to achieve parasympathetic results is far from new. Professional ear-pickers in China have used pressure, tuning forks, and ear-tickling methods for centuries – a dying national pastime that has a very calming effect.
Vagus Nerve Damage
Vagus nerve damage leads to many different symptoms, as this is a long nerve that branches off to various parts of the body. The word ‘vagus’ means wandering in Latin and this name gives us an indication of the nerve’s many pathways.
Damage to the cranial part of the vagus nerve can be caused by brain trauma, infection (encephalitis), the aging process, or chronic inflammation. The main role of the vagus nerve within the brain is to provide sensory innervation to the skin of the back of the outer ear and to the membranes of the ear canal. Hearing disorders such as tinnitus are not caused by CN X but seem to improve when the nerve is stimulated. Sinus infections and dental procedures can produce ear pain as they lie close to the vagus nerve.
Referred pain from, for example, late-stage throat cancer, can also cause pain in the ear region as a result of nerve damage further down the line. Lyme neuroborreliosis and tick-borne encephalitis are both caused by tick bites; a tick bite can lead to acute or chronic forms of brain infection in a small percentage of victims and attack the peripheral nerves, including the cranial nerves.

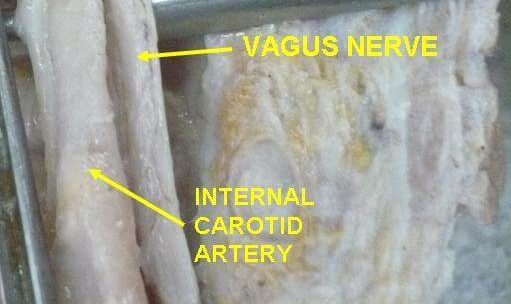
The part of this nerve that passes through the neck can be damaged by trauma, for example during surgery. It is quite exposed as it runs alongside the internal jugular vein and carotid artery before splitting into a right and left pathway just above the aortic arch. Between its exit from the cranium and this right and left splitting of ways, the vagus nerve plays both sensory and motor roles in the neck region.
Damage in and close to the neck can lead to a reduced gag reflex, hoarseness or loss of voice, trouble with articulation and speech, impaired swallowing, and – as already mentioned – referred ear pain, if CN X is affected.
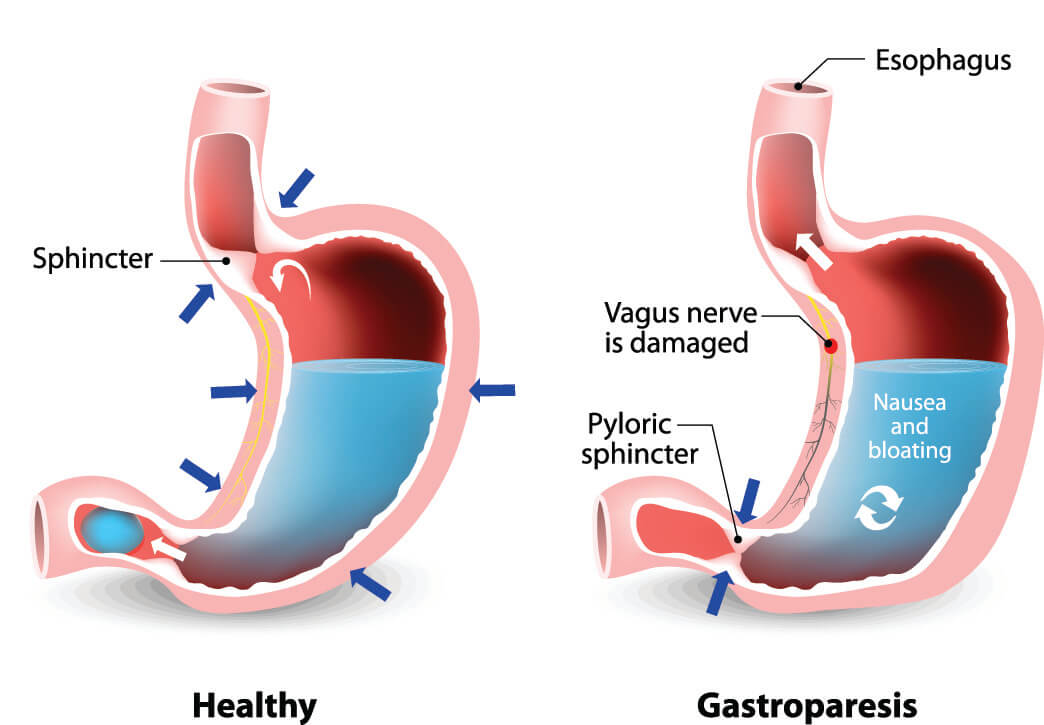
Vagus nerve trauma can also be the result of long-term inflammatory, degenerative, and autoimmune processes. These processes usually affect longer sections with more symptoms such as reduced gastric acid production, irregular heart rate and blood pressure values, nausea and vomiting, abdominal pain, and slow gastric emptying (gastroparesis).
Vagus Nerve Disorders
Vagus nerve disorders are usually the result of lesions or disease and much less commonly a disorder only of the vagus nerve. Tests for vagal damage range from evaluating the swallowing reflex to looking at stomach emptying using computed tomography – a CT scan. An endocrinologist might look more closely at glandular dysfunction associated with vagus nerve damage, and an ear-nose-throat doctor may want to check for infections and tumors.
Nerve diseases can be hereditary or autoimmune. Nerves also degenerate over time, especially in combination with poor nutrition and unhealthy lifestyle habits such as smoking and drinking excessive alcohol. Just like the rest of the body, a lack of blood supply can cause damage to any of the cranial nerves. Metabolic disorders such as diabetes and autoimmune diseases like multiple sclerosis are also associated with vagus nerve disorders; even viruses and bacteria can attack nerve tissue. It has recently been suggested that viral infections of the tenth cranial nerve might be responsible for disorders such as chronic fatigue syndrome, post-traumatic stress disorder, and attention deficit hyperactivity disorder; however, multiple theories can be found all over the Internet and evidence points to there being no singular cause.
