Definition
Staphylococcus aureus is a gram-positive, round (coccus) bacteria found in grape-like (staphylo) clusters; opportunistic colonies cause extreme harm. Staphylococcus aureus is, in limited populations, a commensal bacterium that neither harms nor helps the body. When colonies grow, the bacteria can cause skin, blood, lung, heart valve, brain, and bone infections. Many strains are resistant to treatment with common antibiotics.

Symptoms of Infection
Staphylococcus aureus symptoms only occur when there is excess bacterial growth, such as when our immunity is low and a cut introduces large numbers of bacteria into the blood. Usually, S. aureus bacteria are part of the normal skin and mucous membrane flora (commensal bacteria) and are controlled in numbers by the presence of other commensal bacteria. If conditions suit staphylococci and do not suit the other types of commensal bacteria, S. aureus will colonize the area. In this case, it is an opportunistic bacterial infection. For example, antibiotics that kill other types of bacteria offer a foothold for the opportunistic bacteria that are not affected by the drug, and these take advantage of the situation.
A Staphylococcus aureus infection can be hospital-acquired or community-acquired, colonizing in the absence of a healthy, intact immune system (such as when ill in hospital). Bacteria can be passed on through direct contact with infected people or when in contact with medical staff that unconsciously transmit S. aureus bacteria from instruments and patients to new hosts (cross-infection).
Typical signs of an S. aureus skin infection are even possible when the skin is punctured by a fine needle. These tiny traumatic wounds can become a breeding ground when the immune system is unable to defend the body against pathogenic intruders. Tattoo shops, hospitals, body piercing shops, and injected home medications such as insulin are all risk factors.
A Staphylococcus aureus infection of the skin can enter the bloodstream and colonize in other areas; skin symptoms must be promptly treated. You can spot a staphylococcal skin infection – the skin will present with a boil, impetigo (red sores), cellulitis, or staphylococcal scalded skin syndrome (SSSS) that is a skin irritation (most common in babies) caused by released bacterial toxins.

If an S. aureus infection makes you vomit, you probably have food poisoning. Staphylococcal food-borne disease (SFD) is extremely common, caused by the toxins that these bacteria produce. Enterotoxins (toxins in the gut) produced by S. aureus are the cause of sudden symptoms like nausea, abdominal cramps, vomiting, and diarrhea. As with most types of opportunistic infections, most victims are elderly, very young, or immune-compromised.
Once Staphylococcus aureus enters the bloodstream, where it lands and colonizes decides which symptoms appear. When it colonizes in the bones, septic arthritis with associated joint swelling, pain, and fever can occur. If both the bone and bone marrow are affected (osteomyelitis) the results, if left untreated, are low blood cell counts that cause anemia (low red blood cells), low immunity (low white blood cells), and irregular blood clotting (low platelets). Osteomyelitis is most commonly caused by a cross-infection during joint replacement surgery or in the presence of an open fracture.
Cases of toxic shock syndrome (TSS) caused by S. aureus toxins include symptoms such as high fever, palm and/or sole redness with peeling, muscle pain, nausea, abdominal pain, and even confusion. Although toxic shock syndrome is often associated with postoperative infections, in women the use of tampons is often the culprit, especially when tampons are left in place (or forgotten) for days or weeks.
Septicemia (blood poisoning) is also the result of the toxins produced by all types of bacteria, but S. aureus bacteremia is the most likely to cause death. Bacteremia describes the presence of bacteria in the bloodstream. The toxins they release makes the blood vessel walls leak; this means that the circulatory system becomes much less efficient.
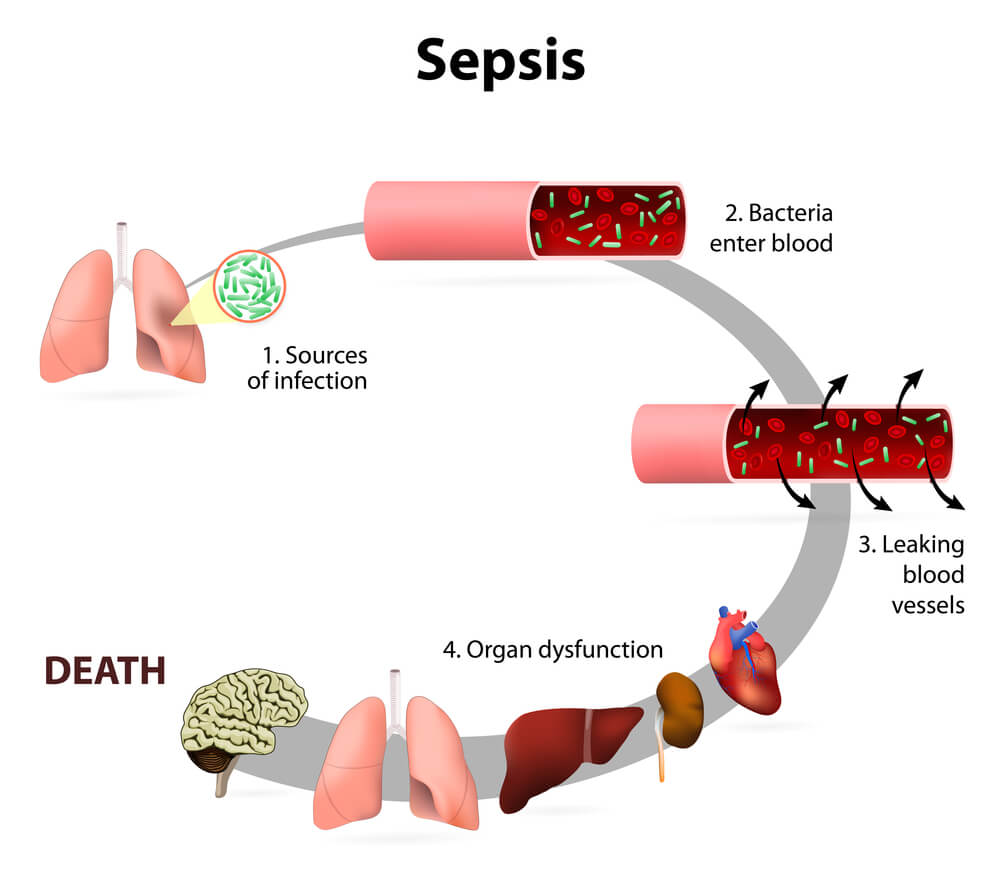
Septicemia triggers a condition known as sepsis – a clinical syndrome that occurs when the immune system response overwhelms the body, causing fever and high numbers of dead cells. This must be in combination with the presence of bacteria and bacteria-produced toxins in the blood. Just to make things plain and avoid confusing the different terms, toxemia only relates to the presence of bacterial toxins in the blood.
Tpxemia is why you may have heard of staphylococcus infections leading to amputation – the blood is so overloaded with toxins that the blood cannot supply the entire body with oxygen. To increase the chances of survival, oxygenated blood is pumped to the vital organs and the extremities (hands, feet, legs) become oxygen-starved.
Septicemia symptoms include high fever, dizziness, and changes in consciousness. Without treatment, septic shock will cause multi-organ failure (MOF) and death. It is estimated that over 1.5 million people develop sepsis every year in the United States alone and of these, around 250,000 dies.
If S. aureus colonizes in the heart, infective endocarditis can damage the heart valves. The most common cause of heart valve replacement surgery in young people is an earlier streptococcus infection. Intravenous recreational drug users are very high-risk populations for heart valve replacement. Damage to the heart valves causes symptoms such as a general lack of well-being, fatigue, coughing, night sweats, spleen enlargement, and can even cause strokes.
Pneumonia as a result of Staphylococcus aureus infection is renowned for its high death rates. The endotoxin Panton-Valentine leucocidin (PVL) is one of the reasons for this. Discovered in around 5% of S. aureus strains, it is a very potent inflammatory regulator that destroys leukocytes (white blood cells) by punching holes in their membranes. This allows the bacteria to grow and increases areas of tissue necrosis (death). Other factors help S. aureus to successfully multiply – the bacteria are often resistant to antibiotics, they can live in the presence of oxygen (aerobic) or without (anaerobic), and they do not die in higher temperatures. Did you know our body’s natural response when infected by bacteria is to cause a fever? The increase in temperature – even by a couple of degrees – can often kill pathogenic bacteria. Unfortunately, this isn’t the case with the staphylococcus species. Infection must be treated as quickly as possible.

Although it is rare, staphylococcal meningitis is an extremely feared condition as its effects can be devastating to the body. Early infection of the membranes that cover the brain usually involves flu-like symptoms and these tend to be ignored. As the colonies of S. aureus increase, symptoms suddenly become more serious. These include skin rashes, high fever, vomiting, double vision, seizures, and changes in consciousness. What staphylococcal meningitis shows is that Staphylococcus aureus bacteria can successfully cross the blood-brain barrier – not every pathogenic bacterium can do this. The National Institute of Neurological Disorders and Stroke regularly updates its Meningitis and Encephalitis Fact Sheet. By knowing how to recognize the symptoms early on, you can save a life.
In staphylococcal meningitis, approximately 21 to 50% of all cases die – young and old. Before the introduction of antibiotics into healthcare, over 80% of cases were fatal. Meningococcal vaccines are available to prevent some other bacterial forms of meningitis but no vaccine has been developed for staphylococcal meningitis, even though it is the most dangerous and rapid-developing type.
Placing urinary catheters without paying attention to hygiene and, in women, the shorter length of the urethra can lead to a whole range of urinary tract infections. These are usually due to Escherichia coli and Klebsiella pneumoniae infections. When S. aureus bacteriuria is diagnosed, the chance is high that this is the result of staphylococcal bacteremia. If the bacteria are found in the urine, it is more than probable that the blood is infected and immediate treatment is required.
Staphylococcus Aureus Treatment
Staphylococcus aureus treatment depends on whether the infecting strain is resistant to methicillin antibiotics (MRSA) or sensitive to methicillin antibiotics (MSSA). S. aureus infections must be treated with antibiotics, especially in elderly, young, and immune-compromised patients. If a prosthesis or any other foreign material such as a urinary catheter, heart valve, or surgical drain is shown to be infected with S. aureus, it must be removed. Prosthetic knee revision surgery rates (due to staphylococcal infection) are approximately one in two hundred in the US.
Hospital-acquired S. aureus is often treated more promptly than cases of community-acquired infection as resistant forms are more likely to be found in hospital environments. Again, MRSA or MSSA testing will determine which antibiotic should be used. Skin infections can be treated topically with antibiotic creams; any boils must be carefully drained. Other infections require oral or intravenous antibiotic therapy, using vancomycin, clindamycin, or a combination of antibiotics for resistant bacterial strains. For non-resistant S. aureus infections, penicillin antibiotics are used.
Staphylococcus Aureus Morphology
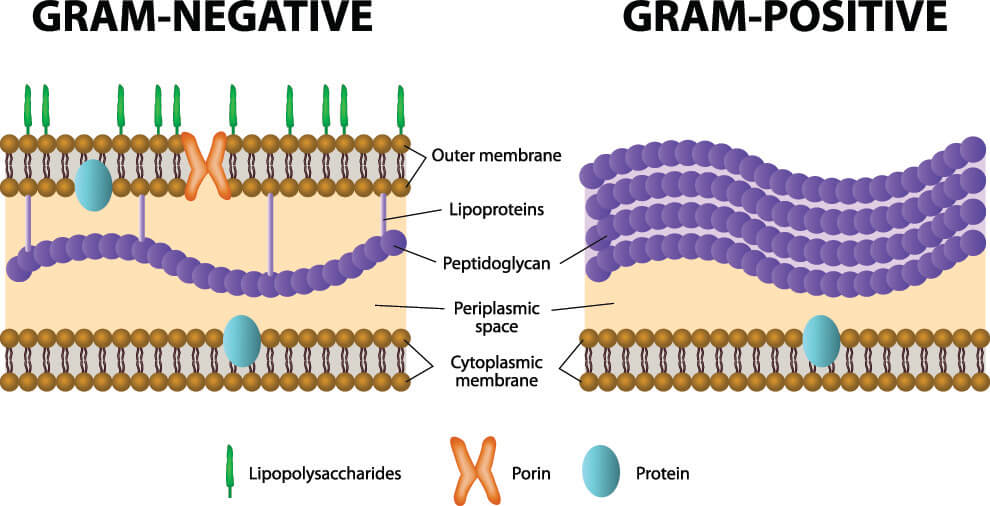
The morphology of Staphylococcus aureus – the shape of the bacteria – if shown under a microscope shows purple clusters of round bacteria. The purple color is not a natural phenomenon but the result of a Gram-stain that colors the thick peptidoglycan membrane of any gram-positive bacteria purple. The natural color of a colony of S. aureus is yellow; in fact, the word aureus means golden. Even though Gram-negative bacteria are traditionally considered to be more harmful, S. aureus kills approximately 20,000 Americans every year.
Unlike other staphylococci, most S. aureus bacteria produce an enzyme called coagulase. This enzyme reacts in the blood to produce another chemical called staphylothrombin. Staphylothrombin might make S. aureus even more difficult to kill by adding a layer of clotted protein to the bacterium membrane. You just have to look at the image below to see how thick the peptidoglycan membrane of Gram-positive bacteria is – an additional layer would make it very hard for a bactericide drug to enter the cell and destroy it.
S. aureus grows both aerobically (with oxygen) or anaerobically (without) at temperatures of between 64.5°F (18°C) and 104°F (40 °C). MRSA strain chromosomes carry a mec gene that can be detected in the laboratory; this test is carried out very early on so that the correct treatment can be immediately started. Early treatment is essential in Staphylococcus aureus infections.
